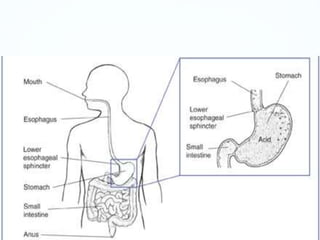
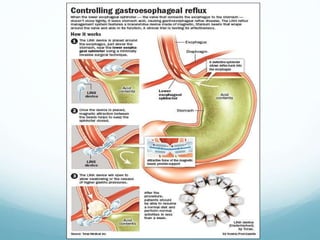
GER occurs when stomach contents backflow into the esophagus. GERD is a chronic form of GER that occurs more than twice a week for several weeks and can lead to serious health issues over time if left untreated. GERD is caused by a weak lower esophageal sphincter or hiatal hernia. Common symptoms include heartburn, cough, asthma, and chest pain. GERD is typically diagnosed through upper endoscopy, pH monitoring, or upper GI series. Treatment involves lifestyle changes, medications like PPIs or H2 blockers, and sometimes surgery. Untreated GERD can cause complications such as esophagitis, strictures, respiratory issues, and Barrett's esophagus