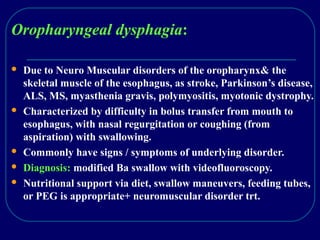
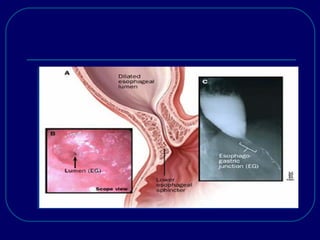
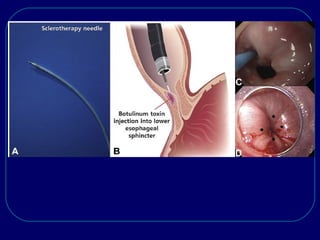
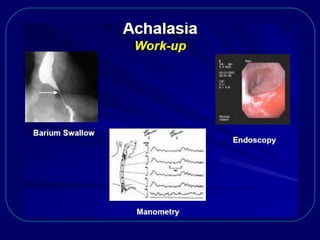
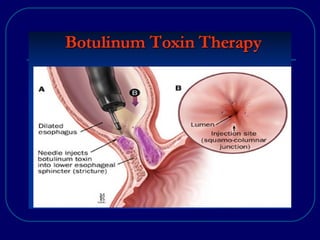
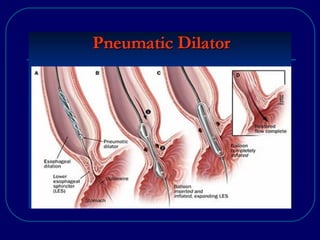
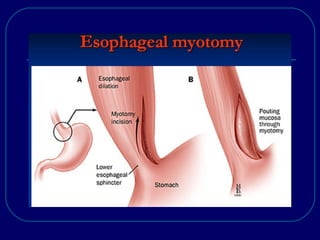
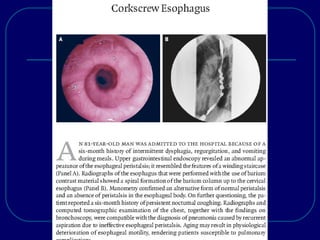
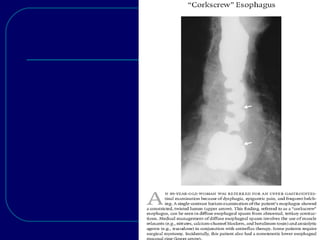
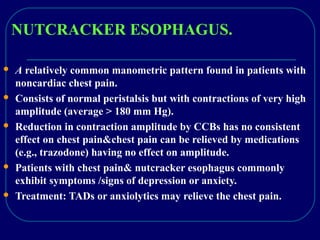
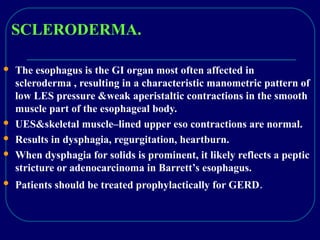
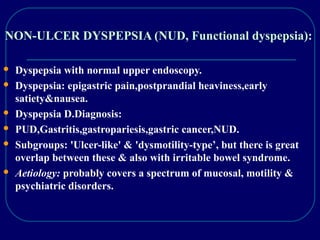
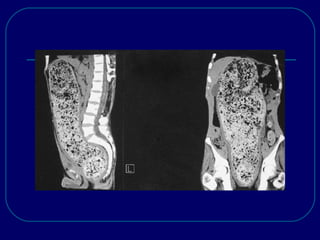
This document discusses various esophageal and gastric motor disorders including their presentation, diagnosis, and management. It covers oropharyngeal dysphagia, esophageal dysphagia from primary and secondary motor disorders, achalasia, diffuse esophageal spasm, nutcracker esophagus, scleroderma, non-ulcer dyspepsia, gastroparesis, and functional vomiting. For each condition, it provides details on symptoms, investigations such as barium swallow and manometry, and treatment options including medications, dilation, myotomy, and nutrition support.