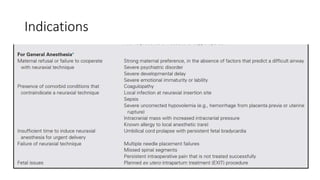
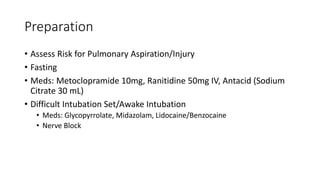
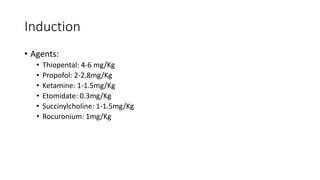
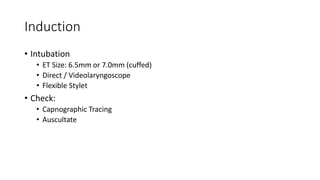
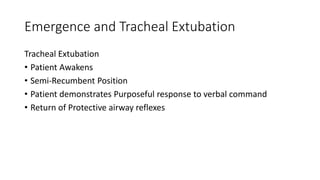
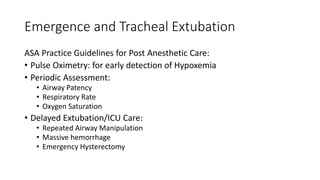
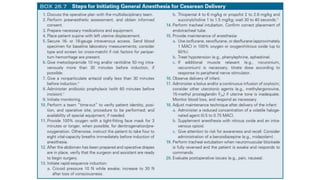
This document discusses general anesthesia for cesarean section, including its indications, preparation, induction, maintenance, and emergence/extubation. It describes assessing risk of pulmonary aspiration and fasting requirements preoperatively. Induction agents include thiopental, propofol, ketamine, etomidate, and succinylcholine or rocuronium. Maintenance goals are adequate oxygenation, normocapnia, minimal effects on uterine tone, and minimal neonatal effects. Agents used are volatile anesthetics at MAC 0.5-1.0, nitrous oxide, propofol, ketamine, and opioids like remifentanil or fentanyl. Extubation criteria include purposeful response