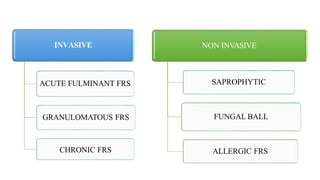
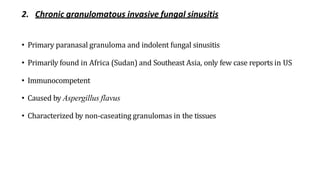
1. Fungal sinusitis can be invasive or non-invasive and is classified based on its histopathological and clinical features.
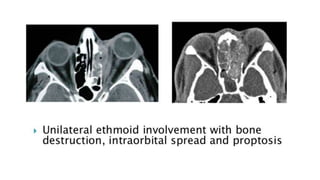
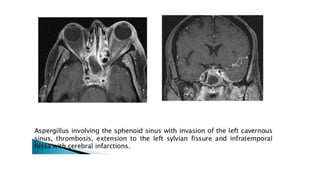
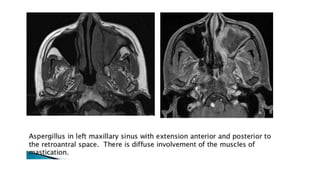
2. Invasive fungal sinusitis includes acute fulminant fungal rhinosinusitis which causes a rapid fungal invasion and is life-threatening with high mortality.
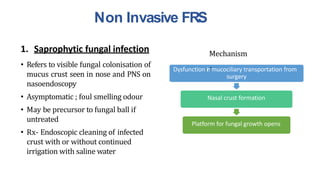
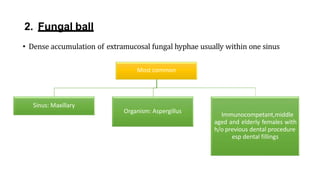
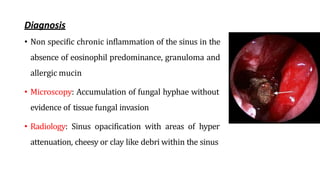
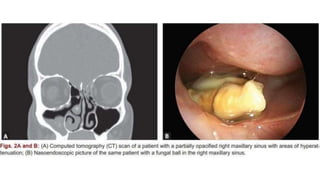
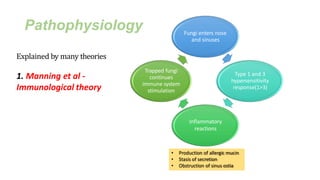
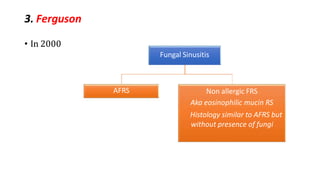
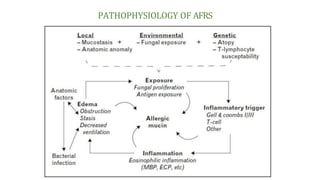
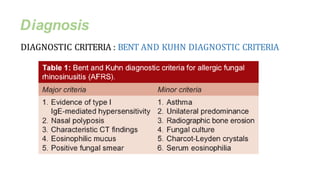
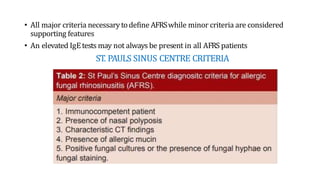
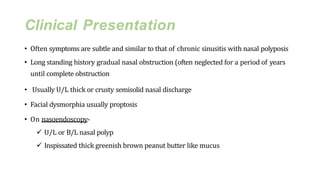
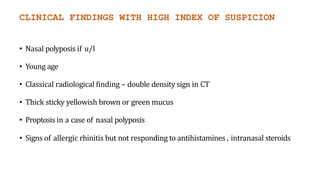
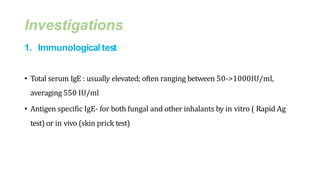
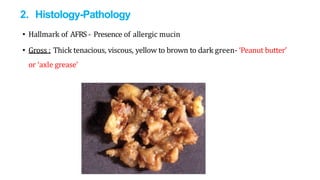
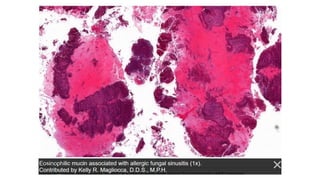
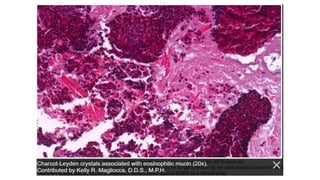
3. Non-invasive fungal sinusitis includes saprophytic fungal infection, fungal ball, and allergic fungal rhinosinusitis which is characterized by eosinophilic mucin containing fungal elements and is associated with type I hypersensitivity.