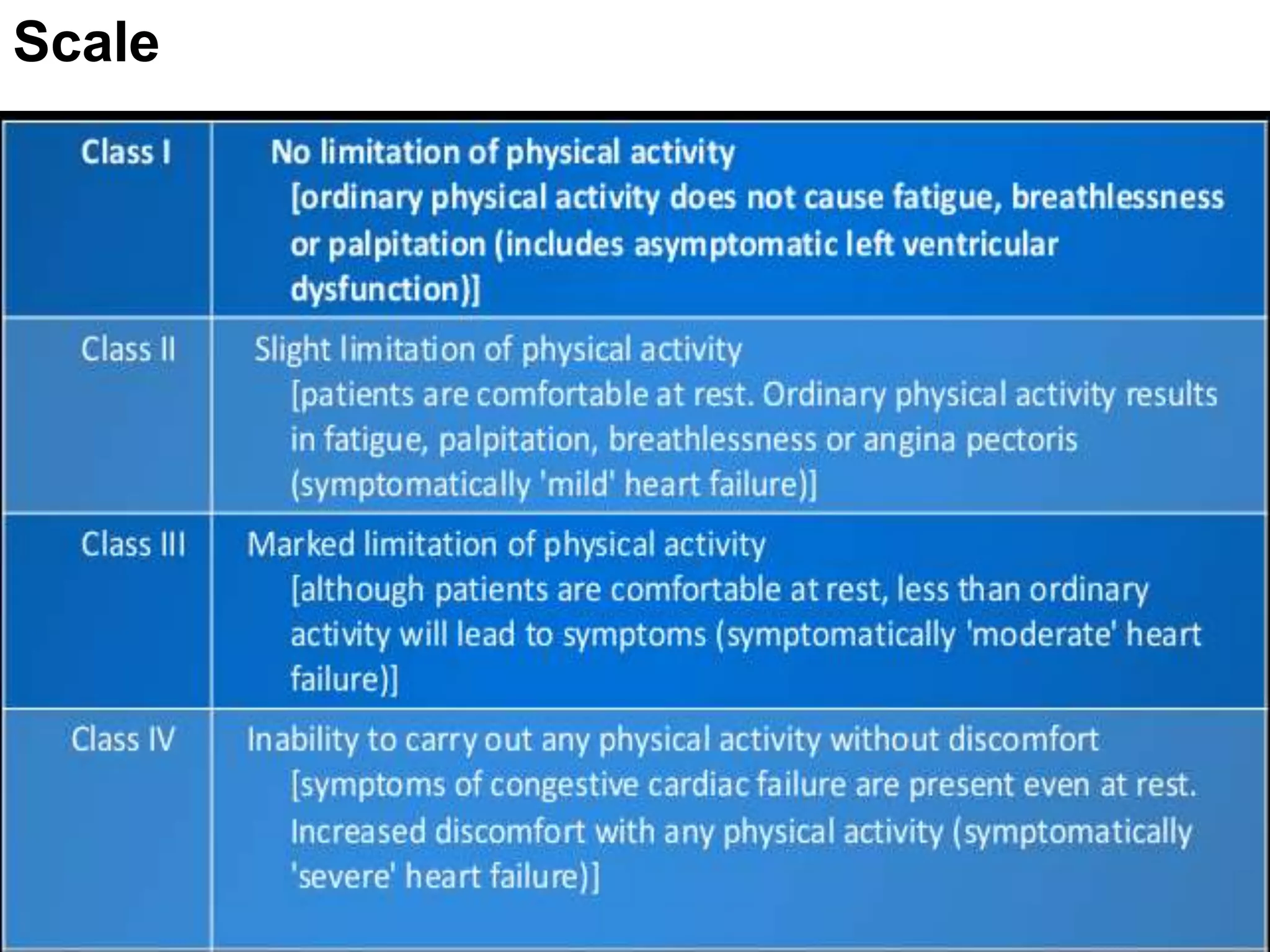
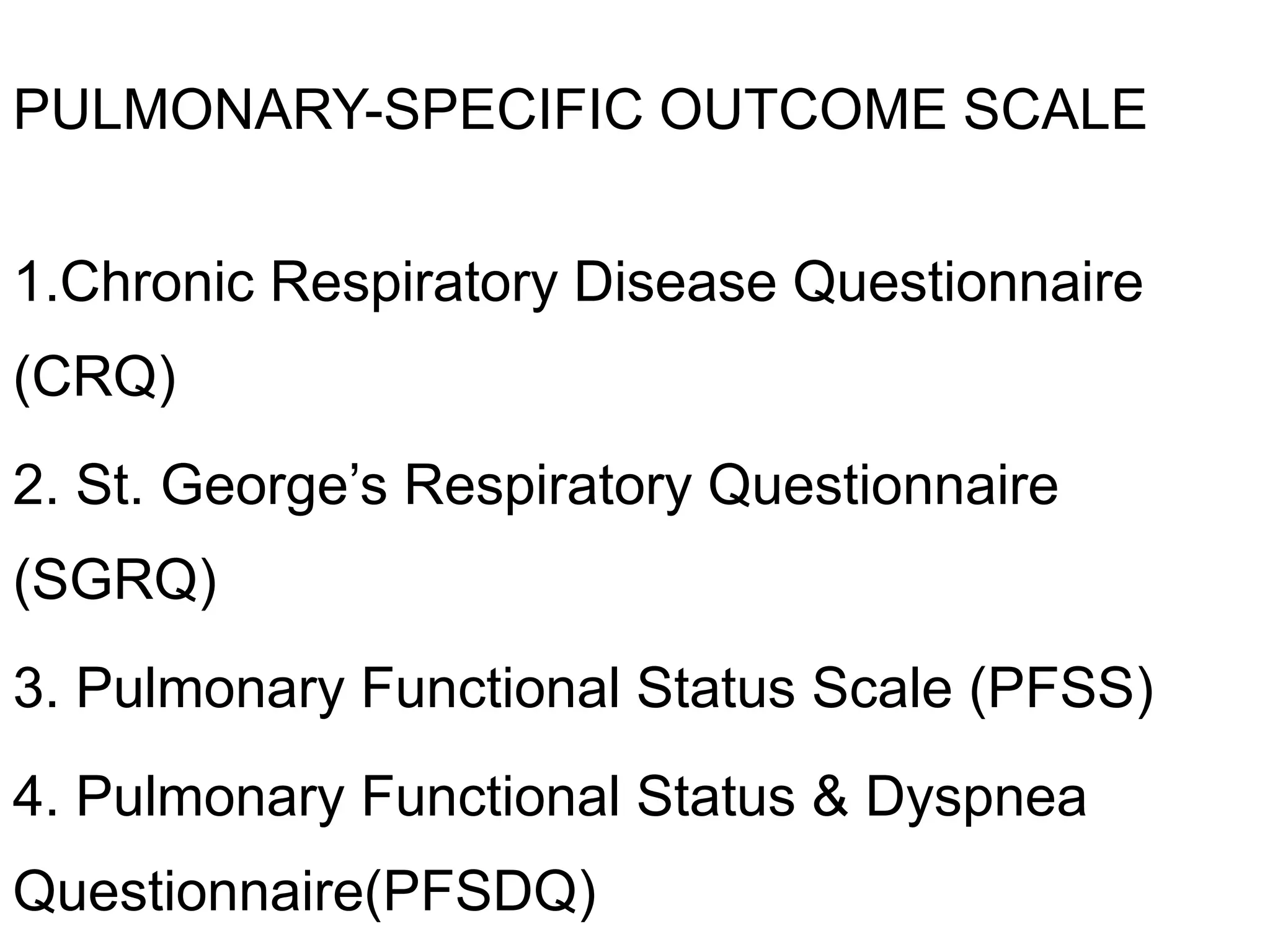
The document discusses the use of functional outcome scales in cardiovascular and respiratory conditions, outlining various tools like APACHE, SAPS, and MPM, which help in assessing patient morbidity and predicting outcomes in intensive care. It emphasizes the importance of these scales for improving clinical decision-making, accountability, and research while classifying them based on cardiac-specific and pulmonary-specific metrics. The document also highlights general quality of life measures to evaluate the overall health perception of patients.