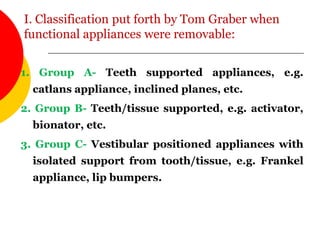
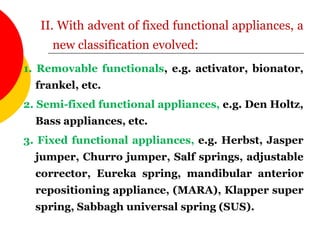
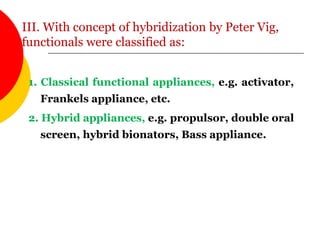
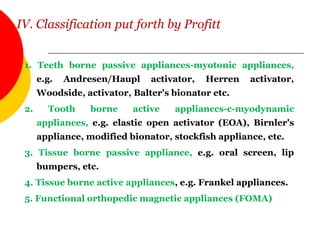
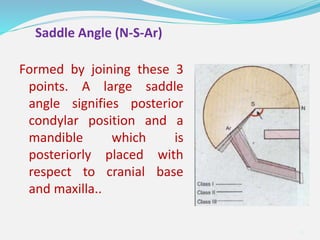
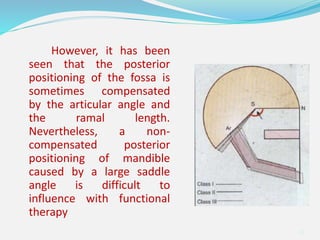
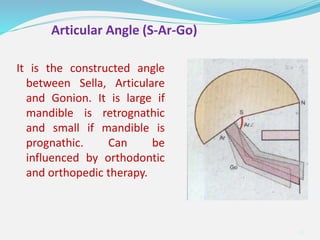
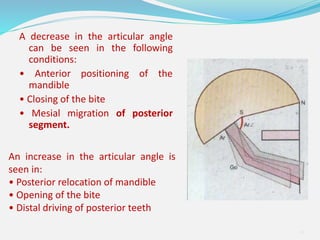
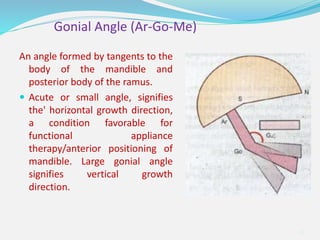
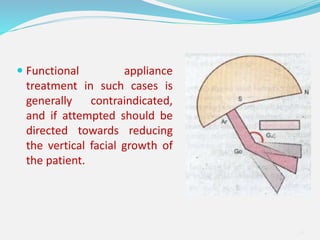
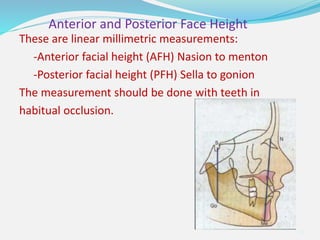
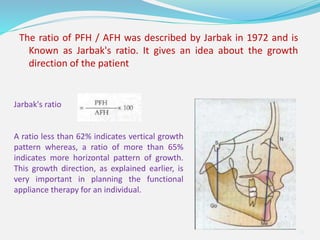
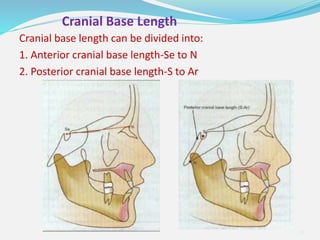
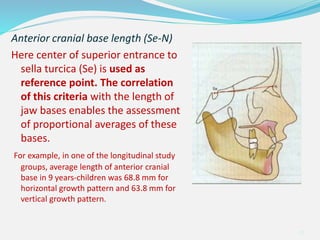
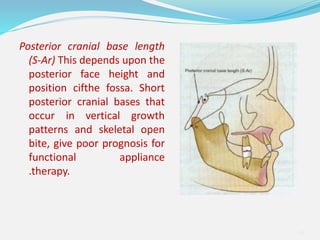
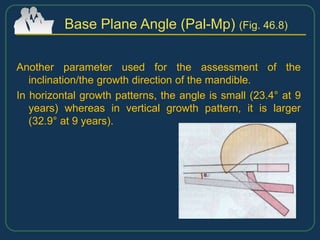
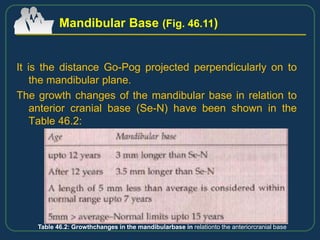
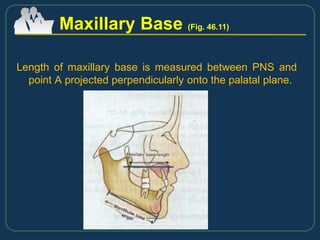
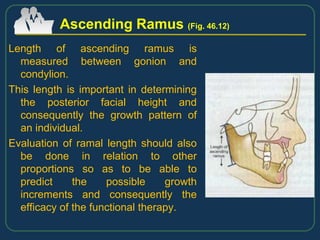
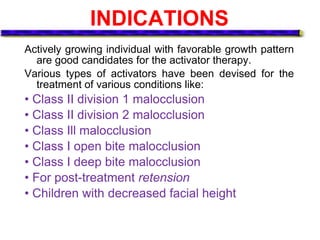
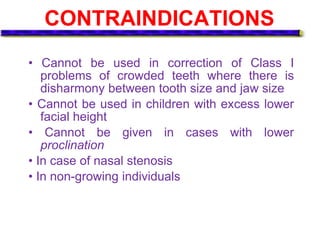
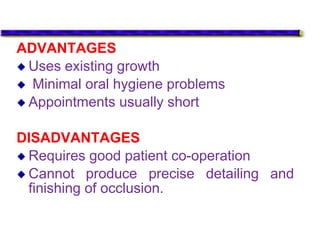
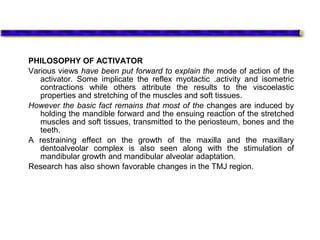
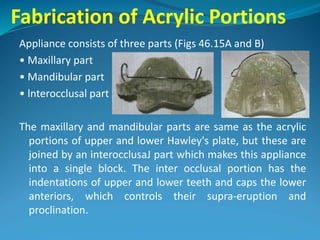
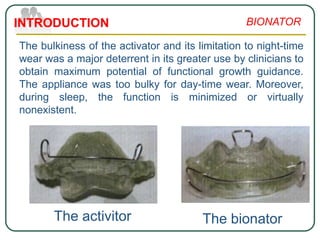
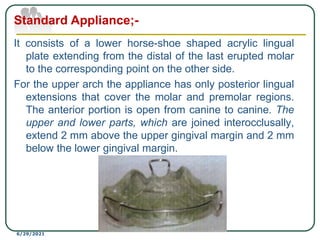
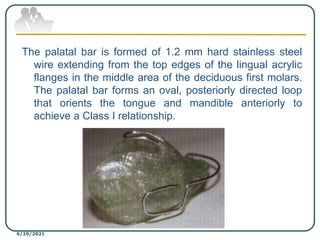
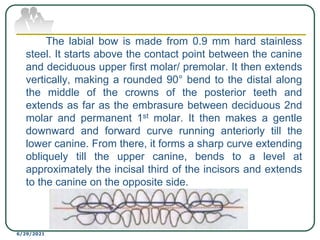
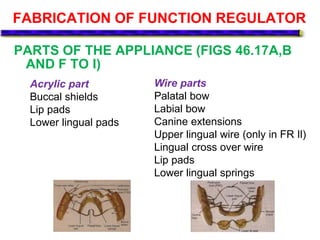
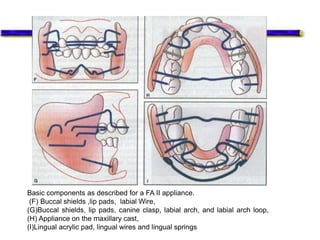
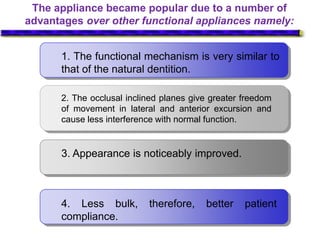
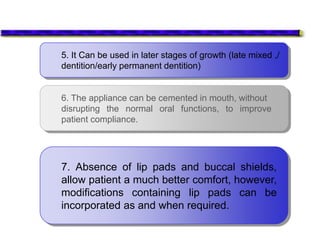
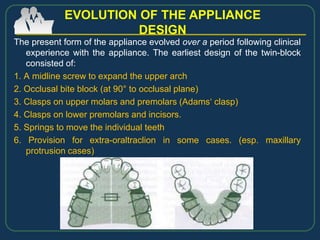
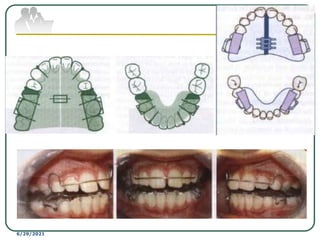
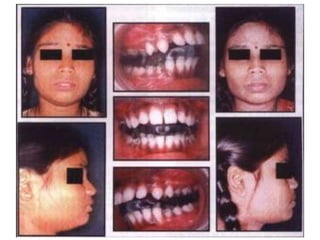
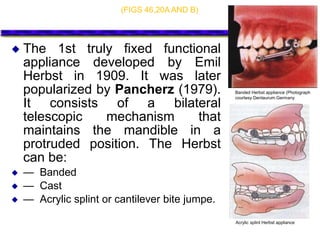
This document provides an overview of functional appliances used in orthodontic treatment. It begins with an introduction to functional appliances and their use in guiding natural forces to correct morphological abnormalities. It then covers classifications of functional appliances, how cephalometric analysis is used to assess patients, and descriptions of common appliances like the activator, bionator, and twin-block. The document discusses how functional appliances can correct Class II and III malocclusions by influencing facial growth. In under 3 sentences.