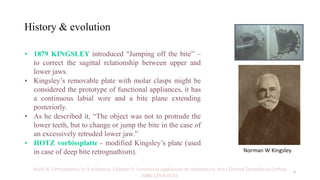
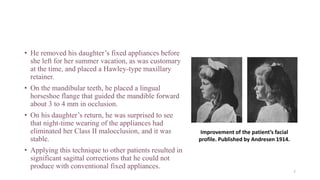
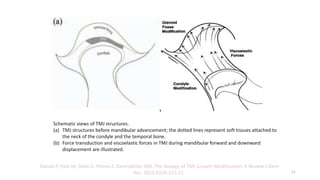
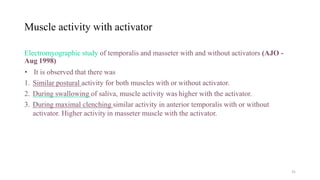
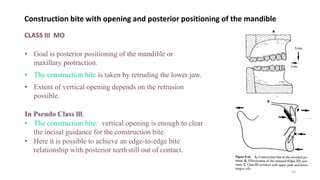
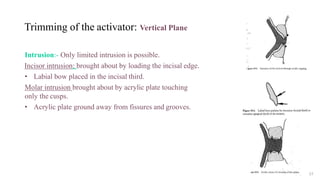
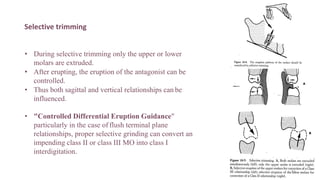
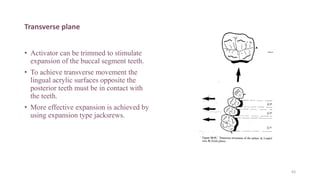
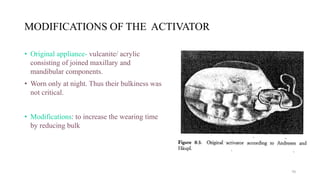
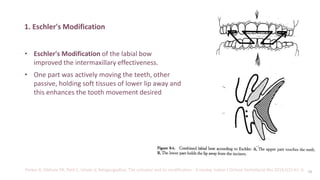
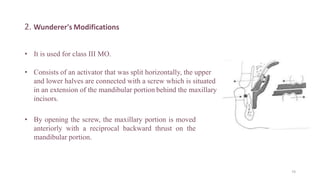
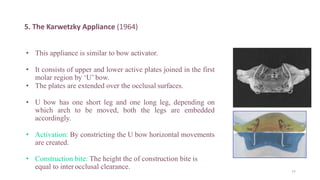
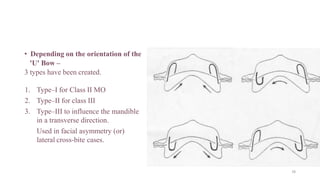
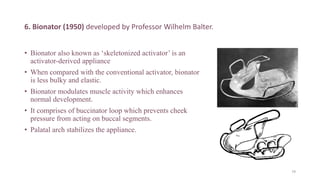
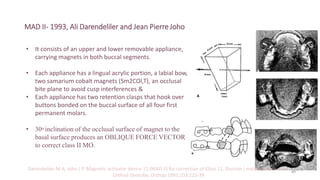
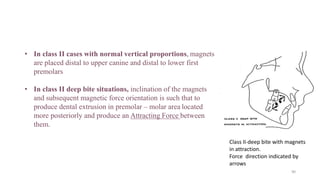
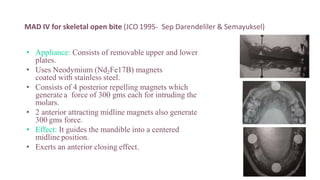
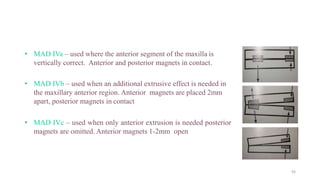
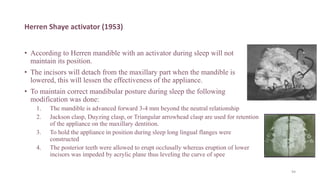
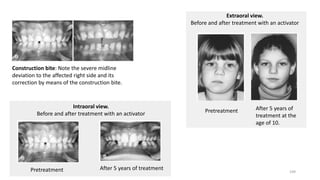
The document provides an in-depth overview of the activator appliance in orthodontics, detailing its history, function, and effects on dentofacial structures. It discusses the principles of activator therapy, including its indications, contraindications, advantages, and disadvantages, along with historical context and clinical applications. Key findings note the activator's role in influencing mandibular growth and correcting skeletal relationships, particularly in growing individuals with specific malocclusions.