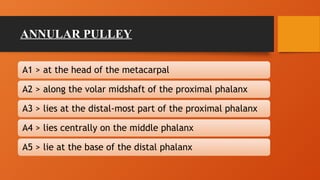
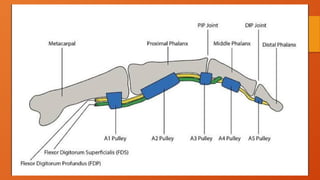
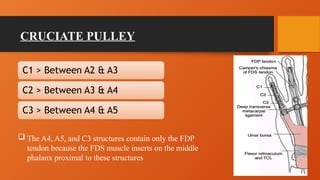
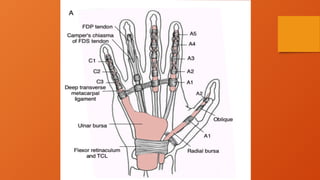
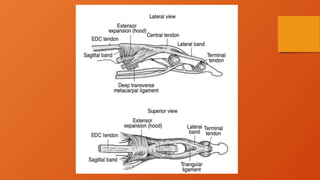
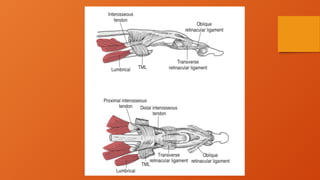
The document discusses the anatomy and function of the flexor and extensor mechanisms of the fingers, emphasizing the importance of structures like pulleys, tendon sheaths, and muscles in facilitating movement and preventing dysfunction. It details how these mechanisms influence metacarpophalangeal joint function and outlines conditions like trigger finger and clawing that can result from their impairment. Additionally, it highlights the intricate relationships and roles of various components involved in finger extension and flexion.