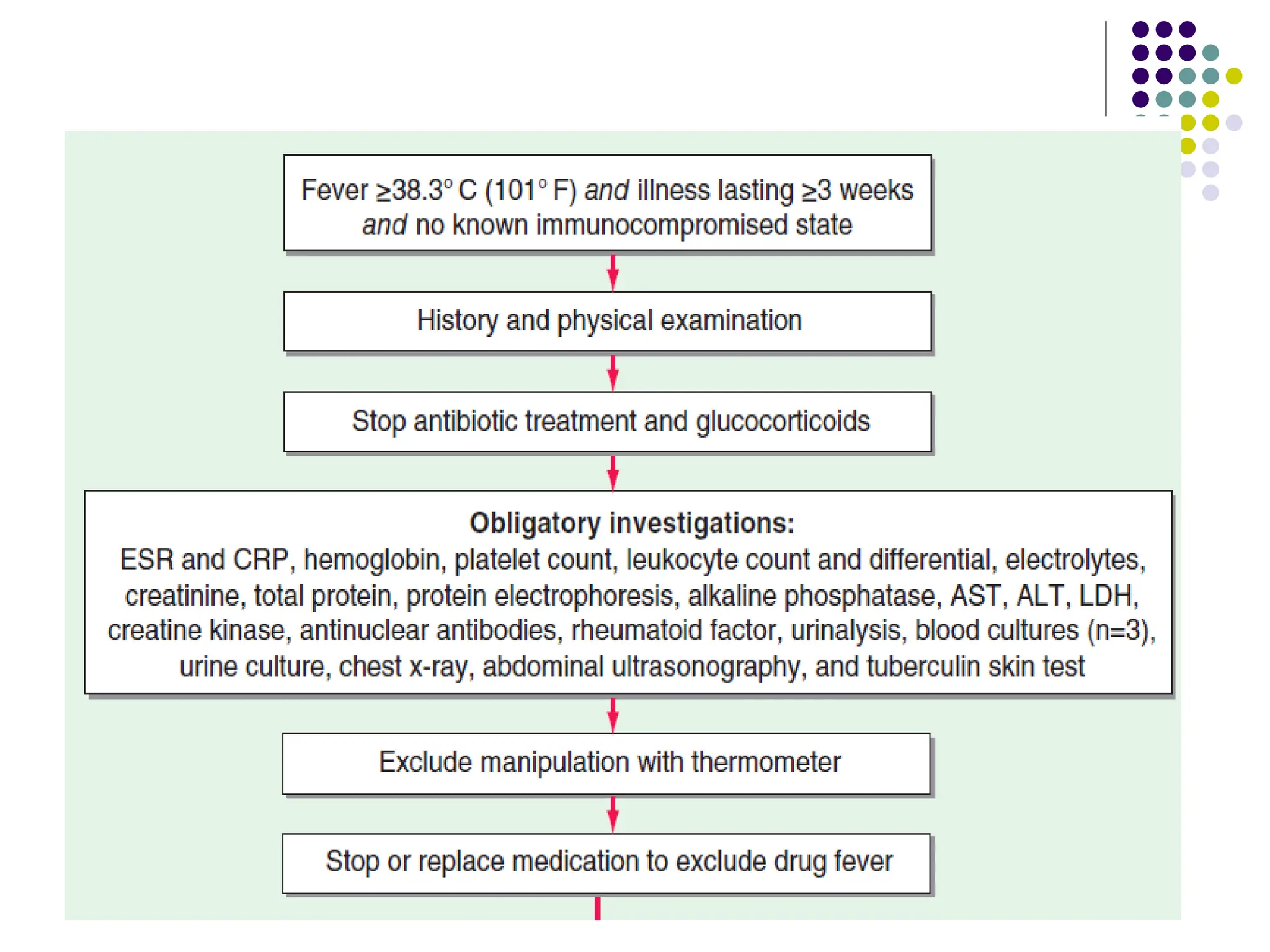
The document discusses the regulation of body temperature and mechanisms of fever, detailing the role of the hypothalamic thermoregulatory center and its response to pyrogens that increase the hypothalamic set point. It elaborates on different types of fever, their effects on the body, and the principles of treatment, highlighting the significance of fever in diagnosing underlying infections or diseases. Additionally, it covers specific considerations for fever in children and the elderly, as well as the classification and etiology of fever of unknown origin (FUO).