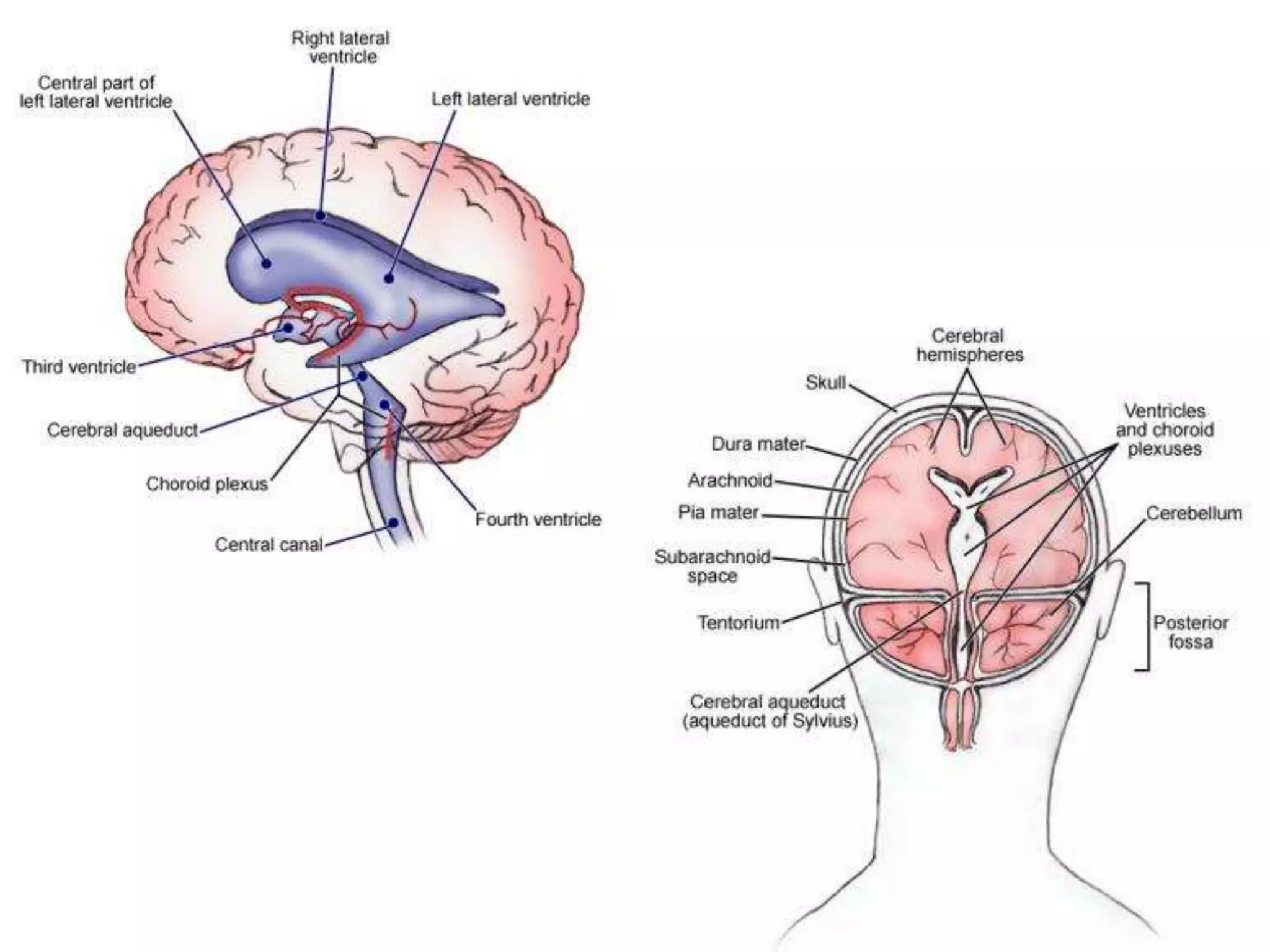
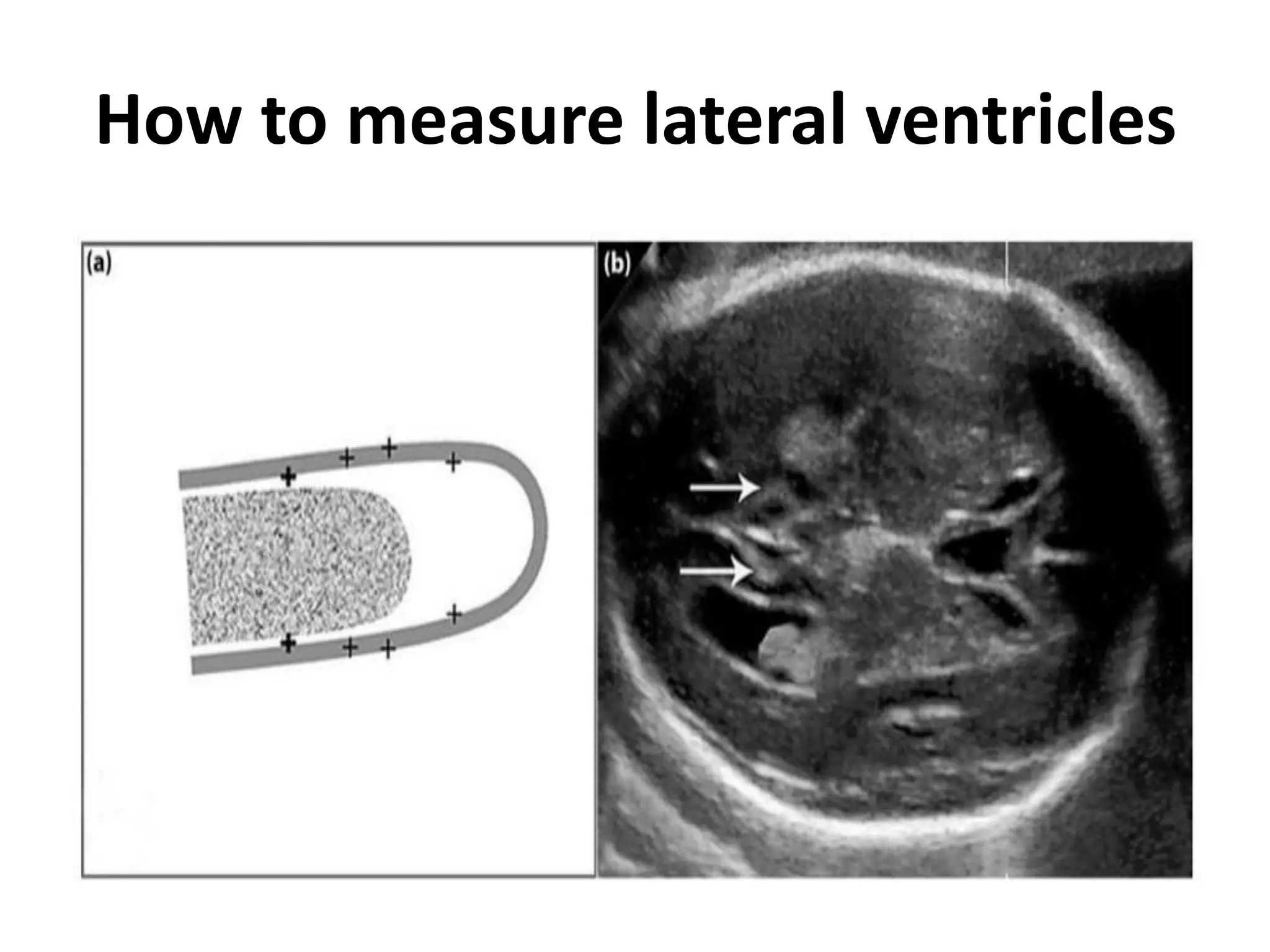
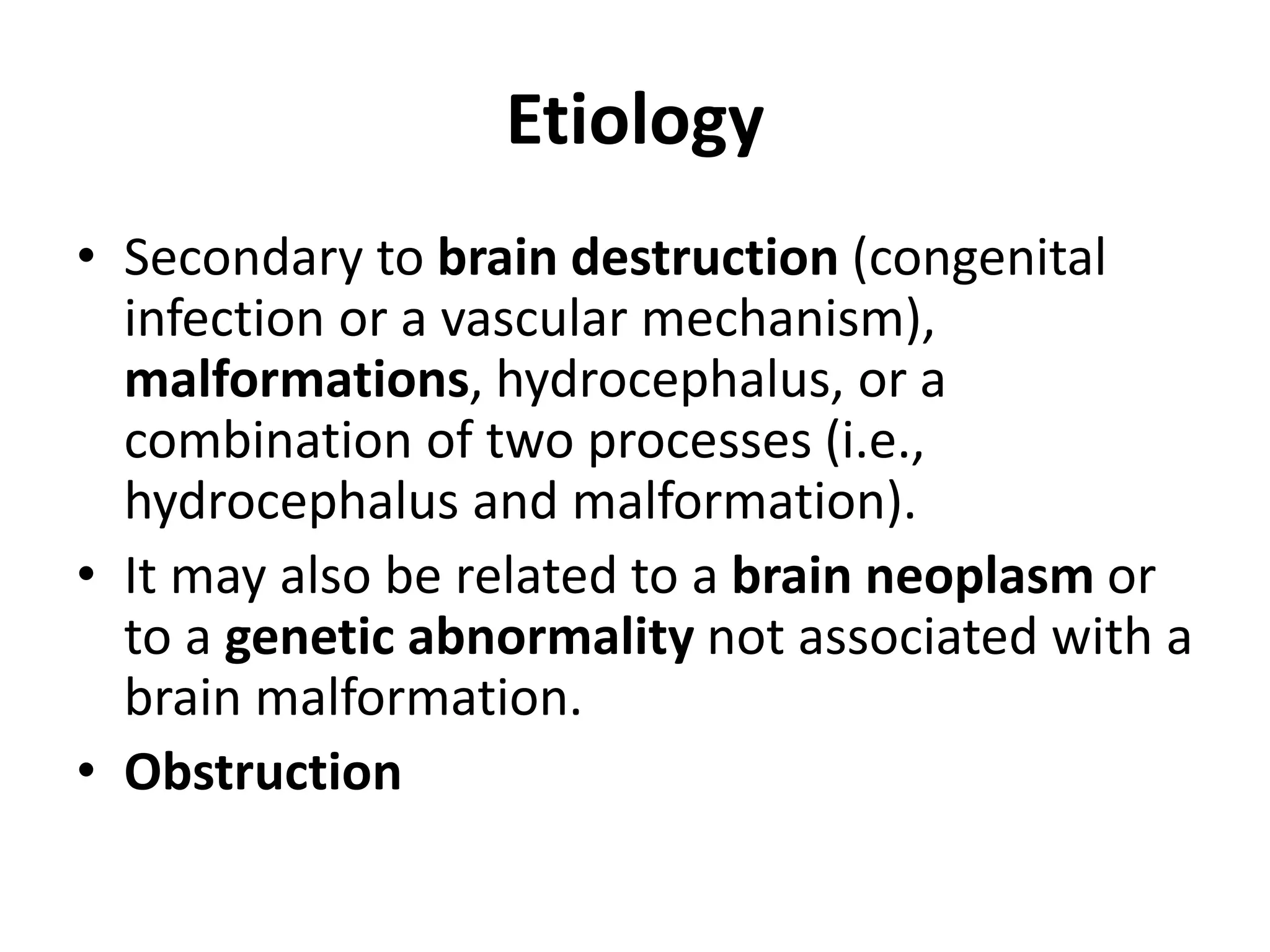
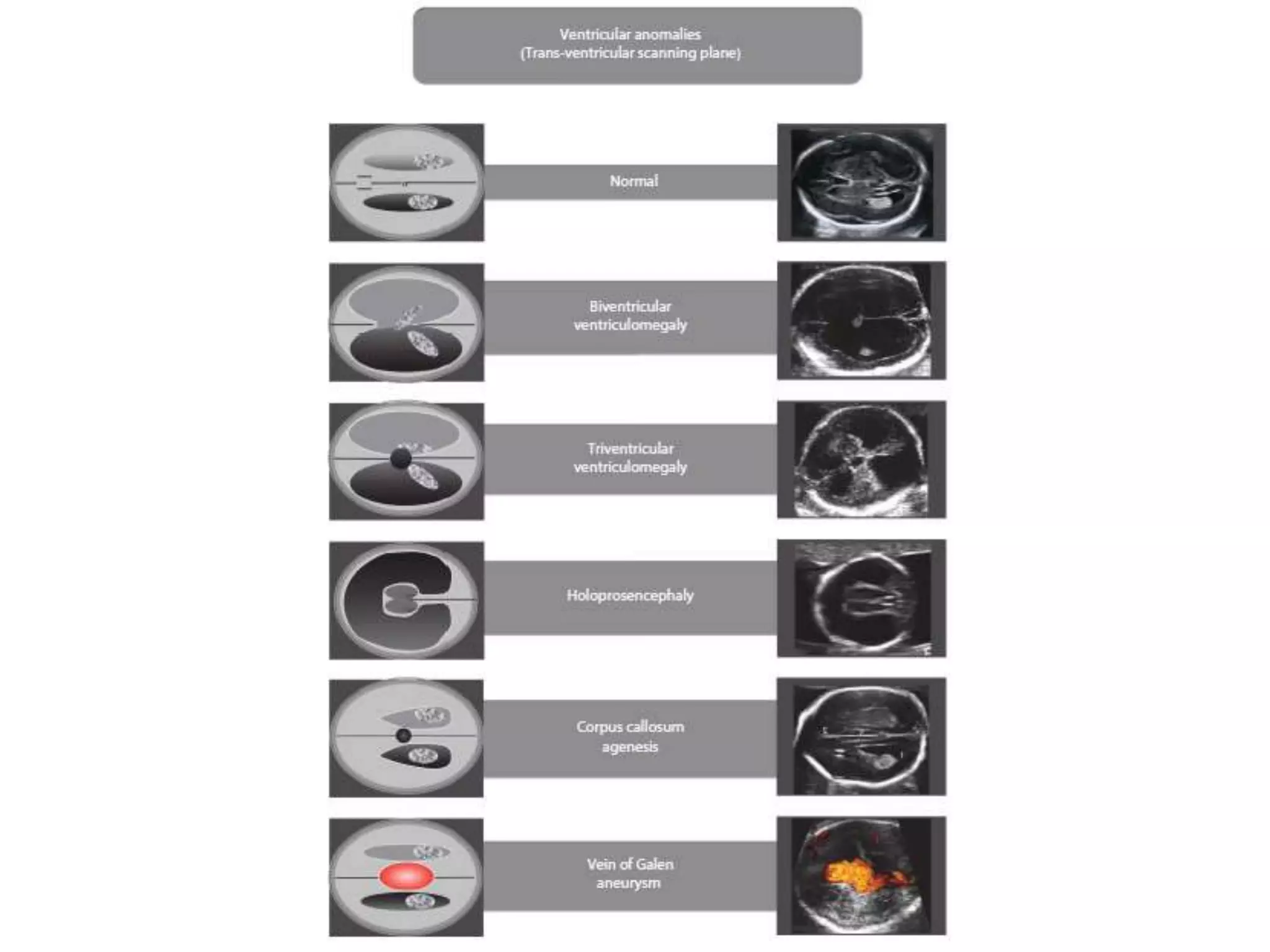
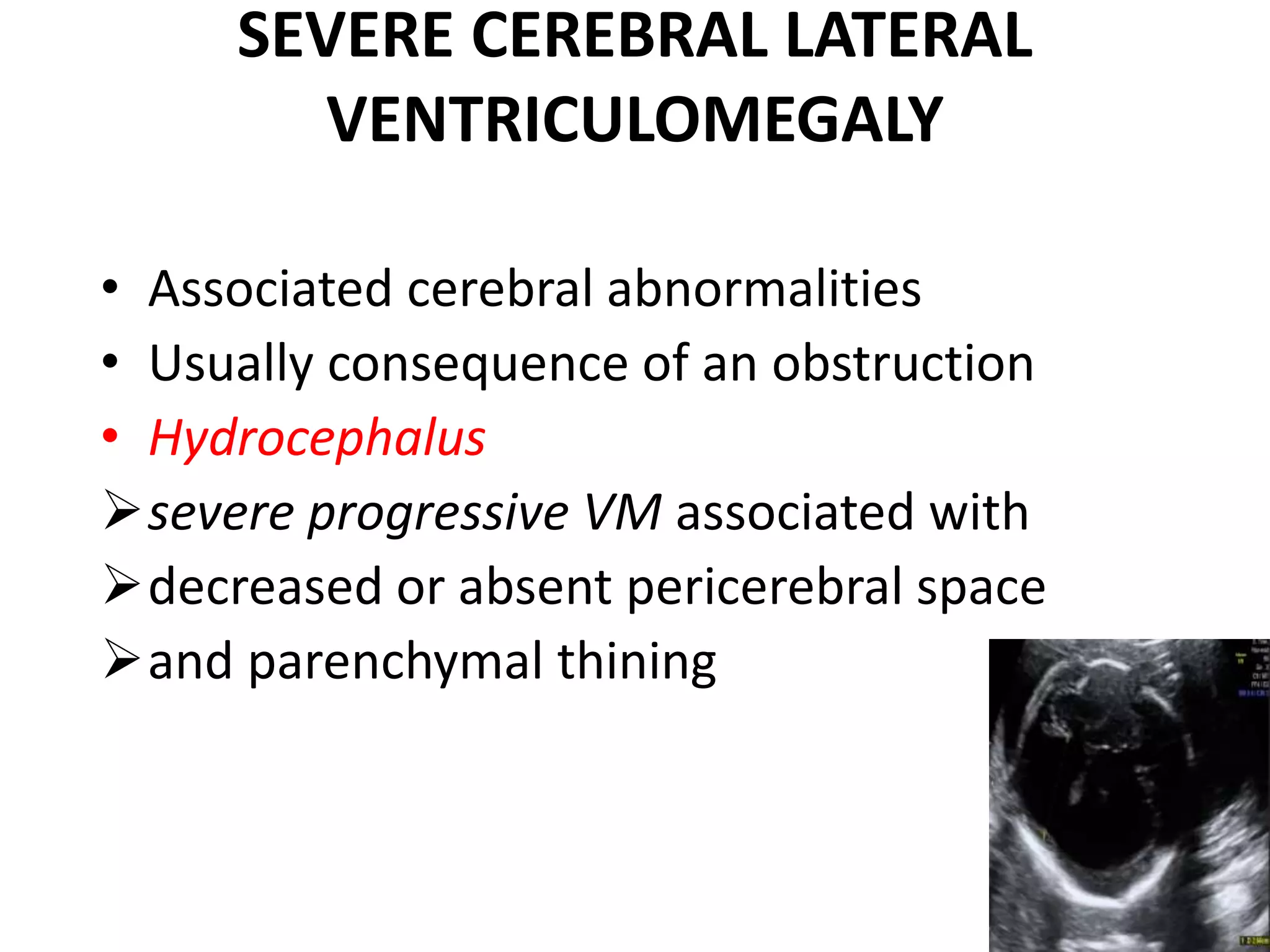
This document discusses ventriculomegaly (VM), which is the enlargement of the lateral cerebral ventricles. VM has many potential causes including infections, vascular issues, hydrocephalus, malformations, or genetic abnormalities. It can range from mild to severe. Evaluation involves detailed ultrasound exams and may include fetal MRI or maternal infection testing. Isolated mild VM carries a low risk of problems while isolated severe VM has poorer outcomes. Recurrence risks vary depending on the underlying etiology.