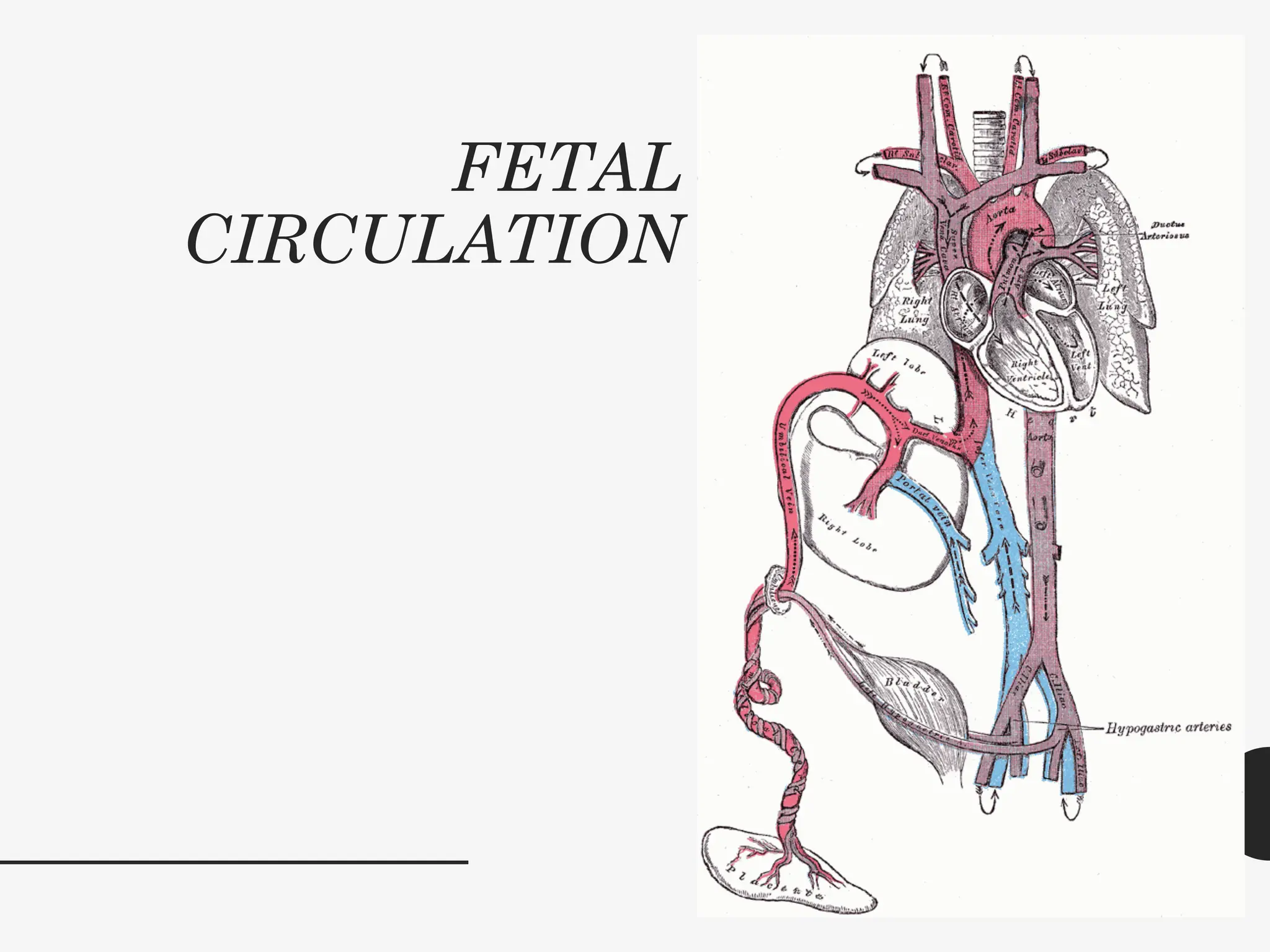
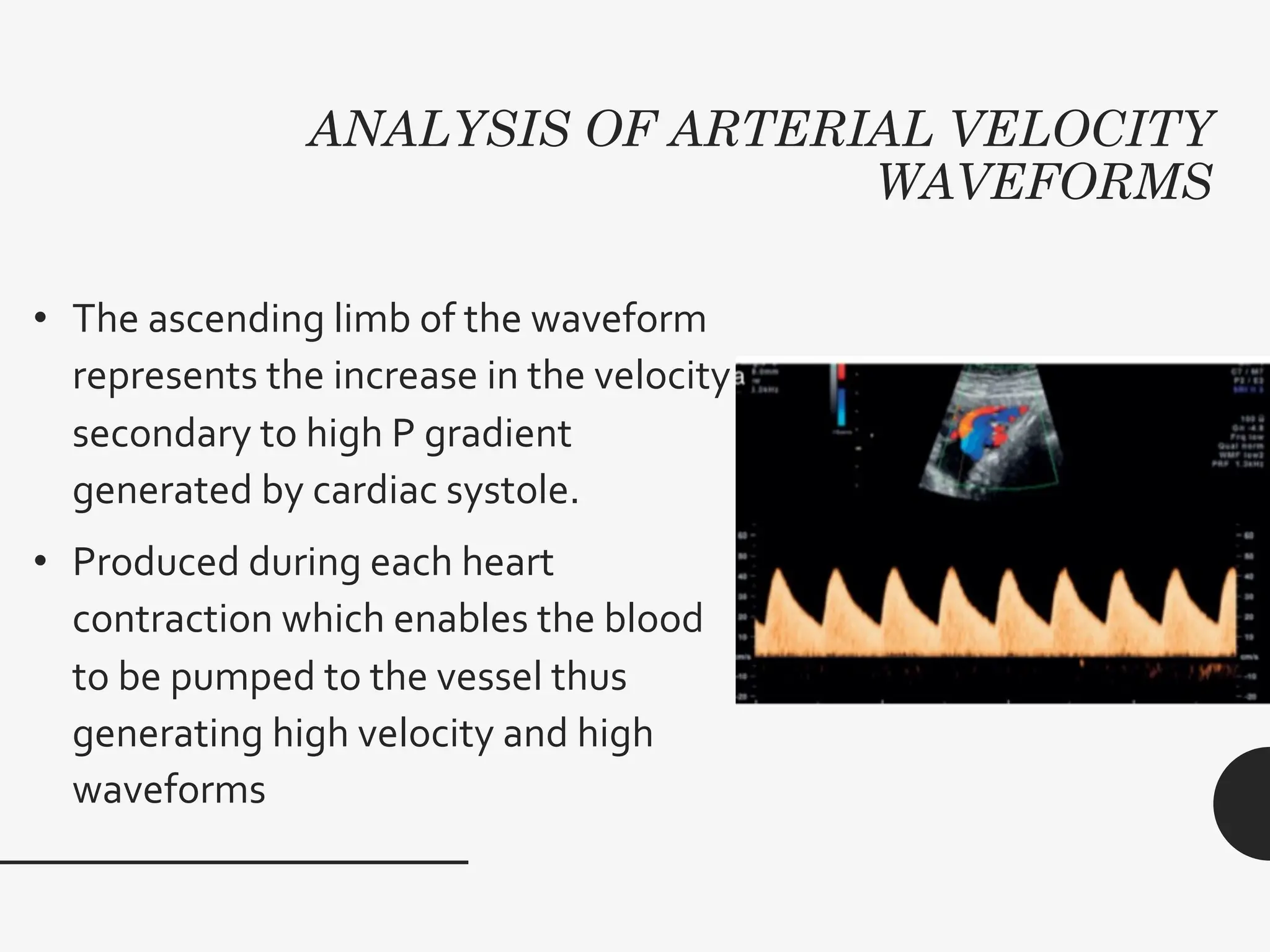
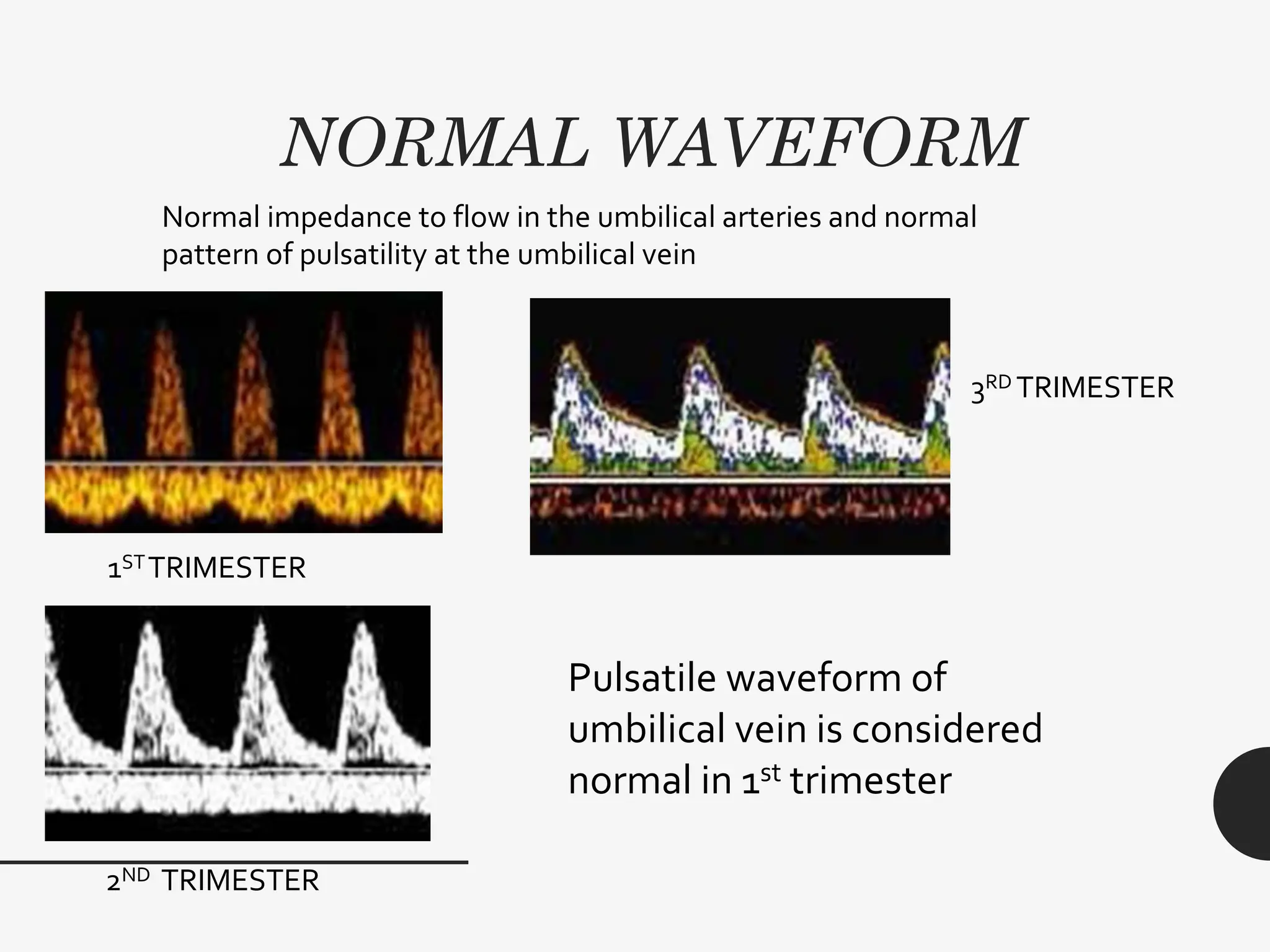
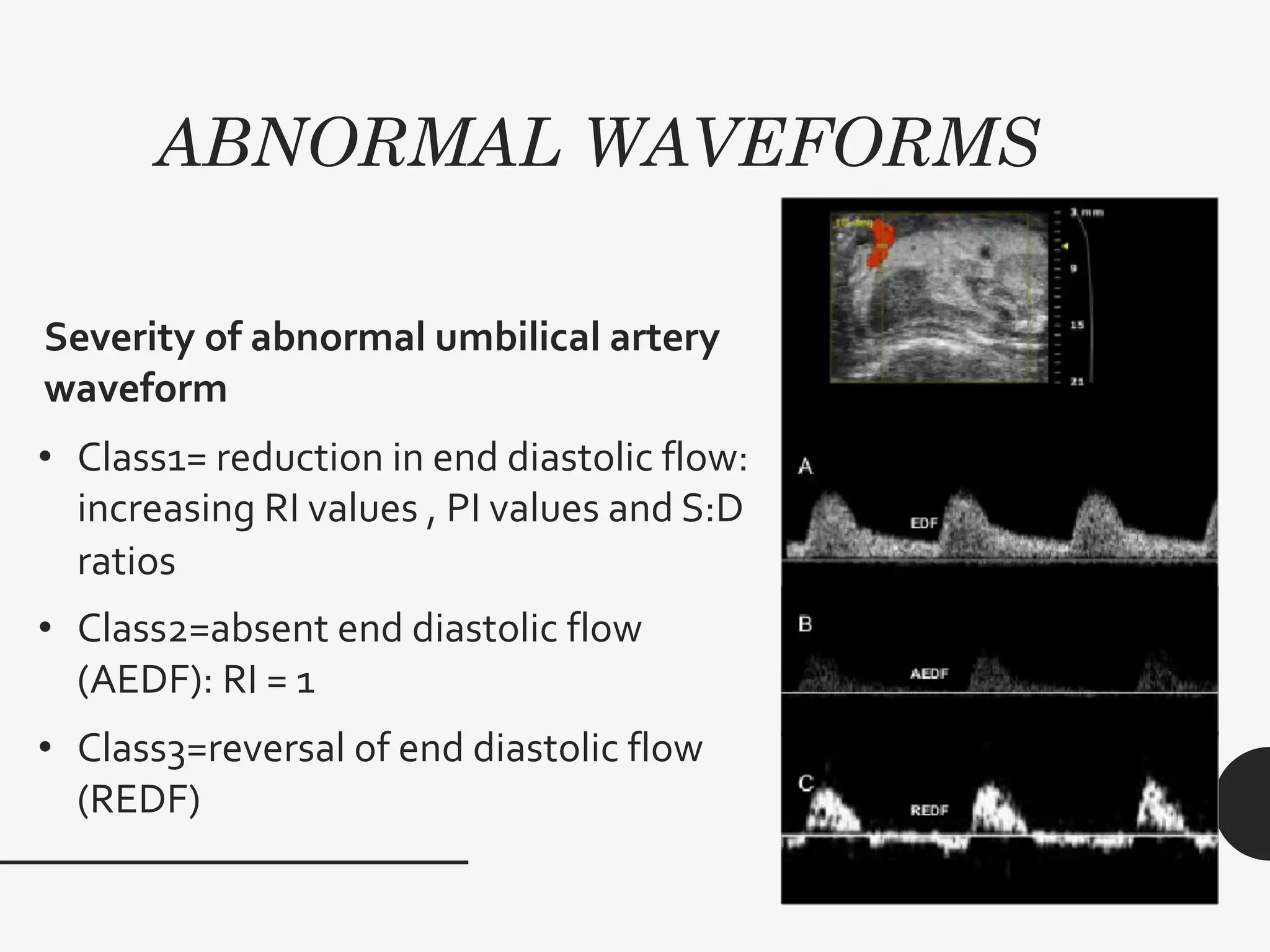
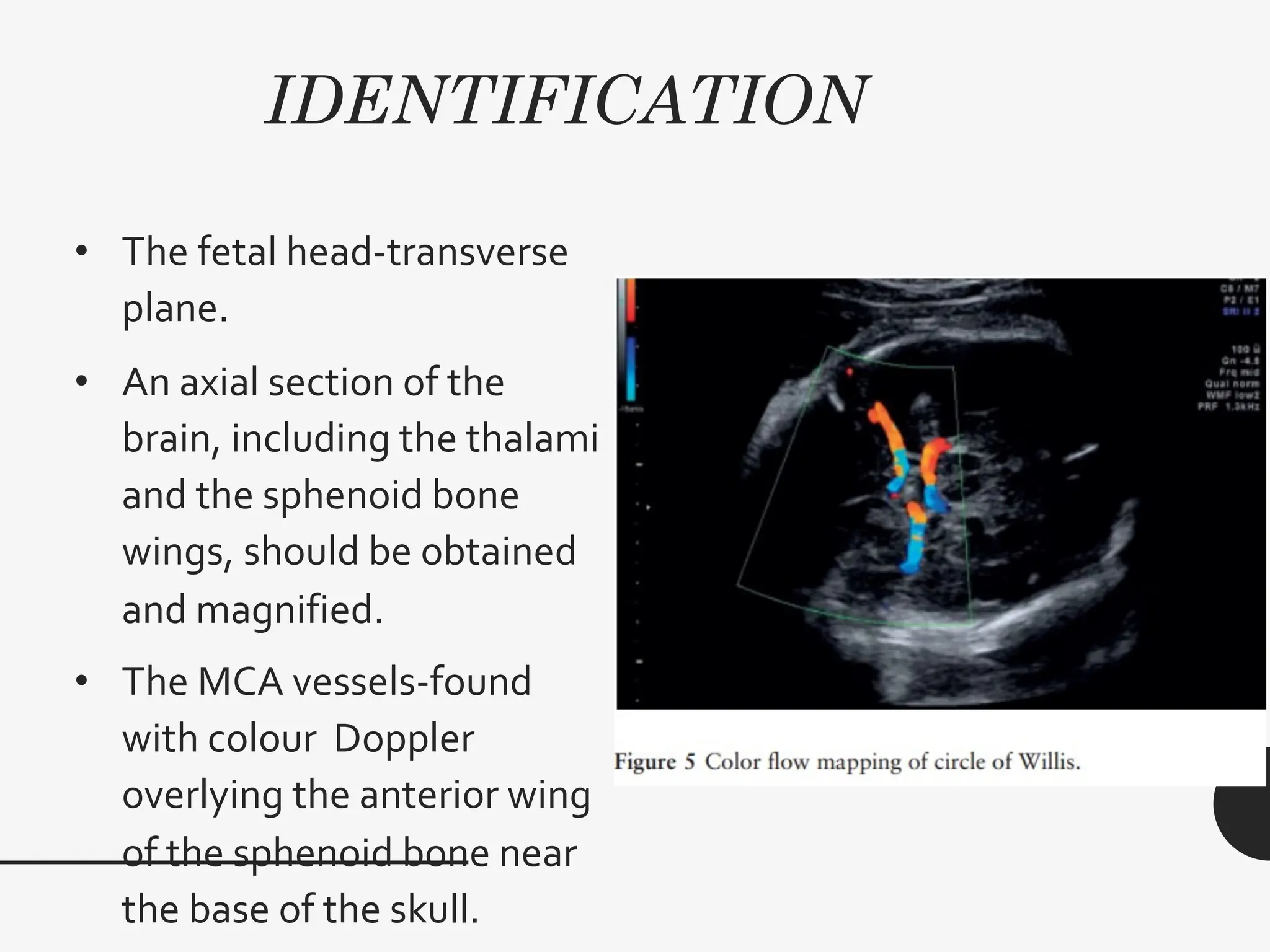
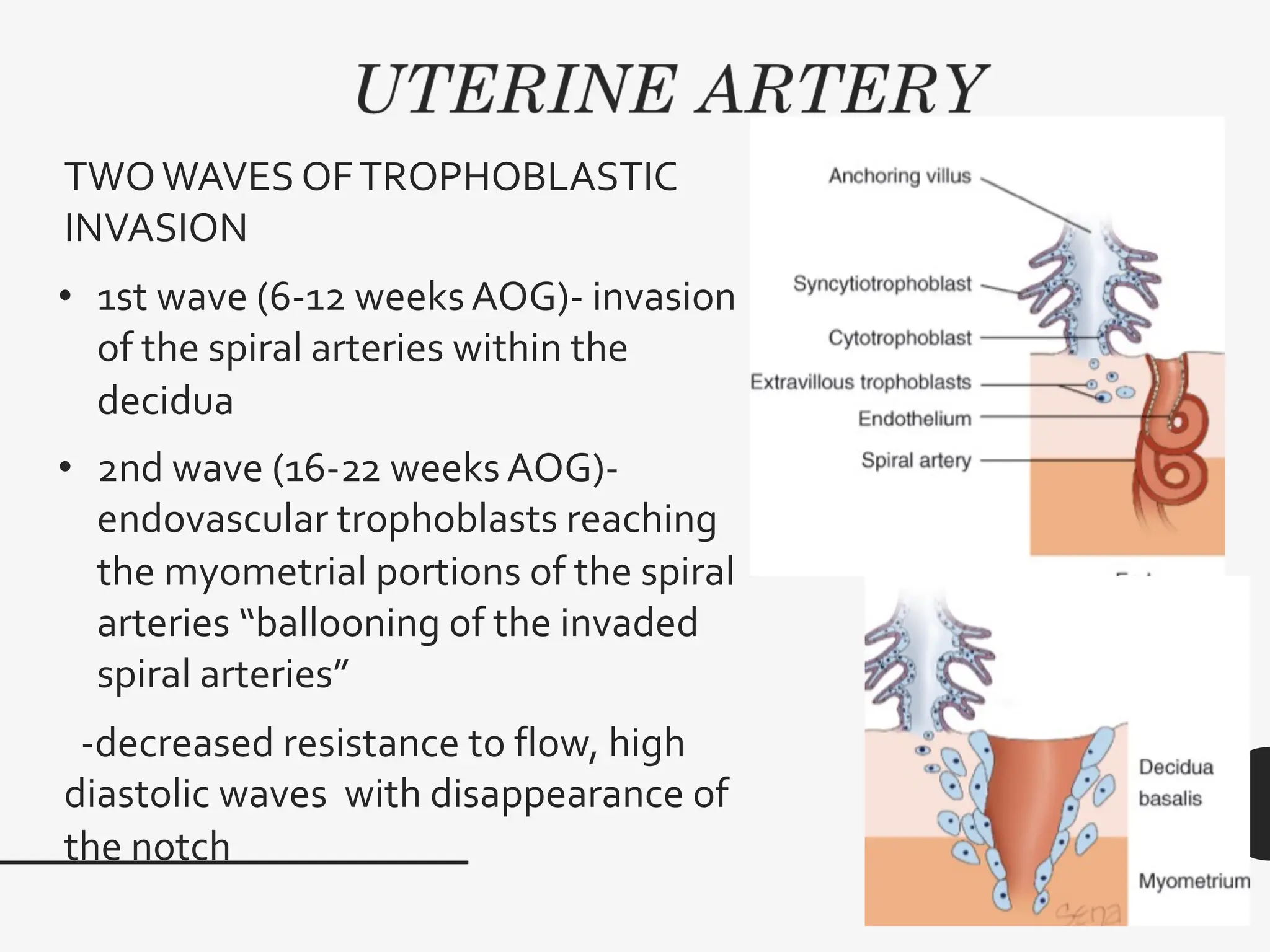
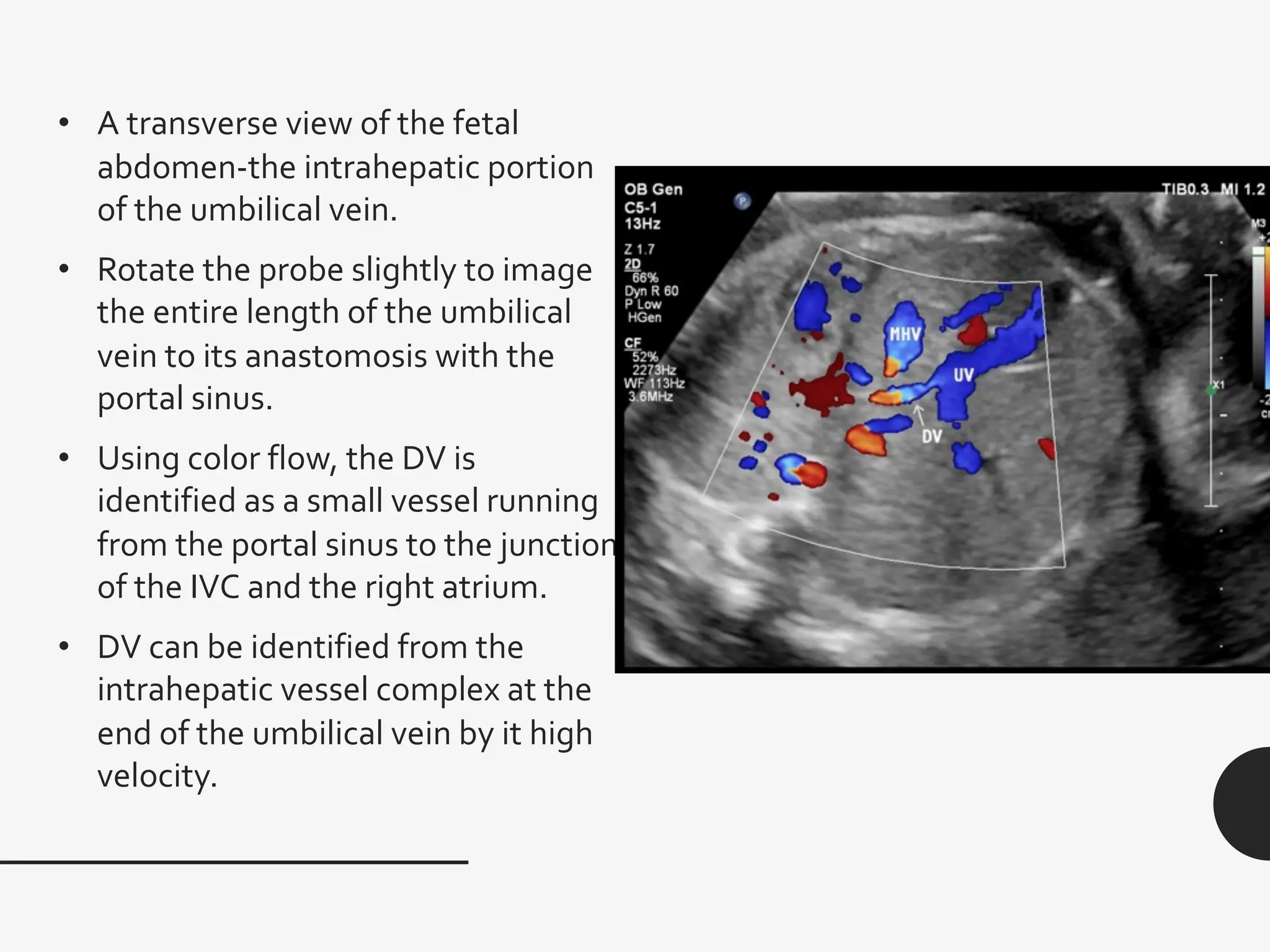
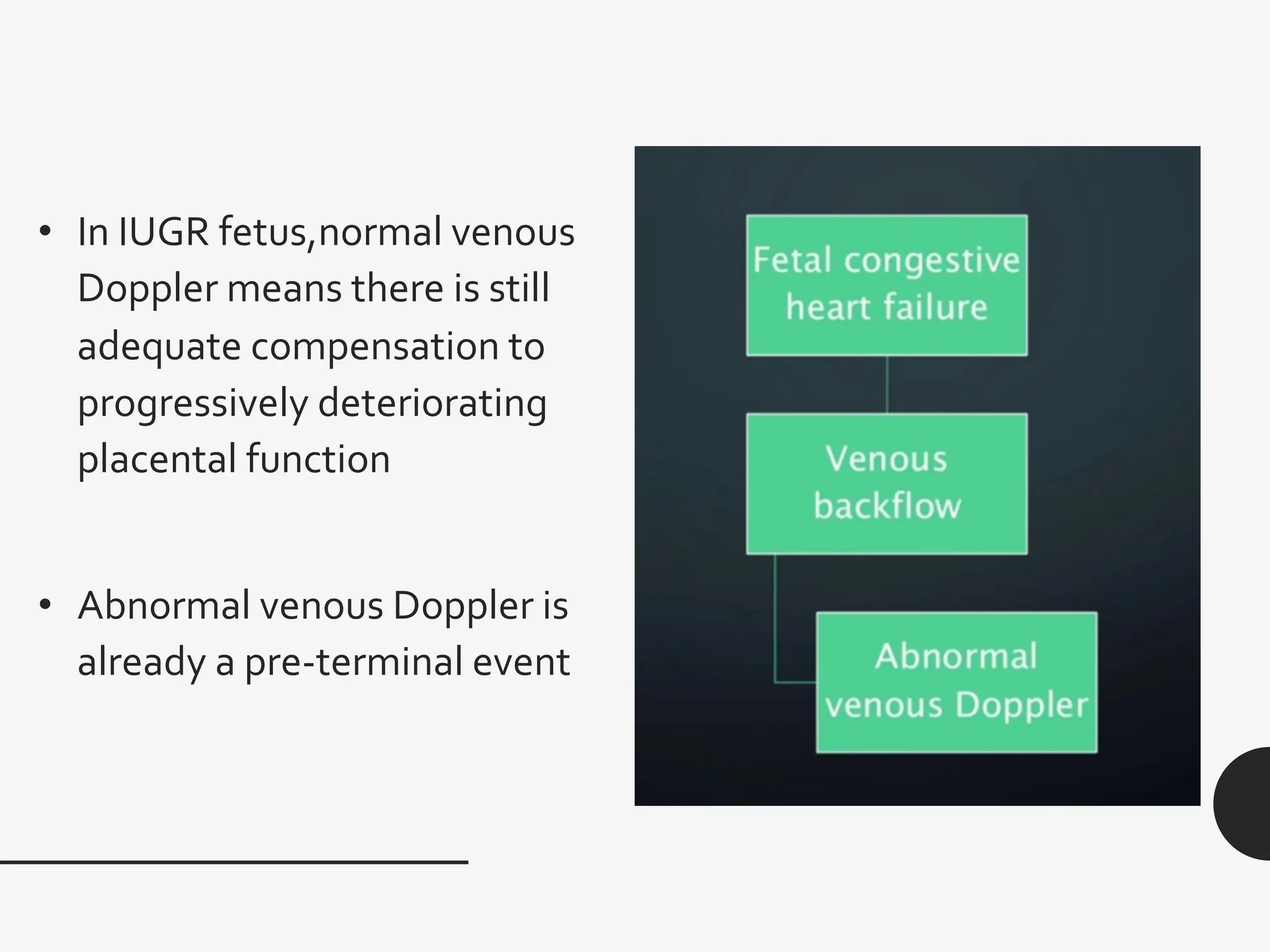
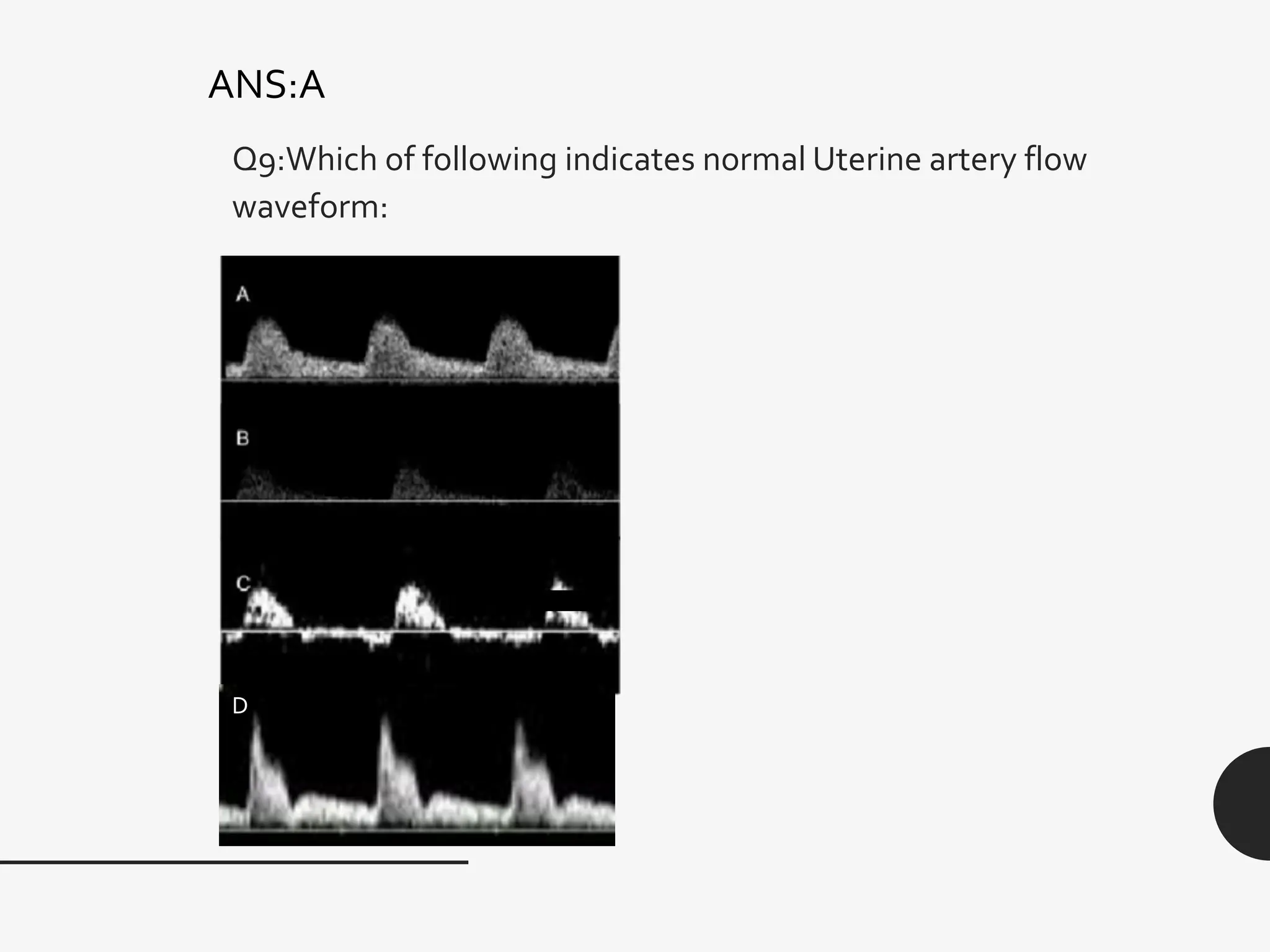
This document provides an overview of Doppler ultrasonography in obstetrics. It discusses the prerequisites for Doppler studies including the ultrasound machine capabilities and patient preparation. It describes the indications for Doppler including fetal growth abnormalities and maternal risk factors. It examines in detail the various fetal and maternal vessels that can be assessed by Doppler including the umbilical artery, middle cerebral artery, and uterine arteries. It outlines the normal and abnormal waveforms seen in each vessel and their clinical significance.