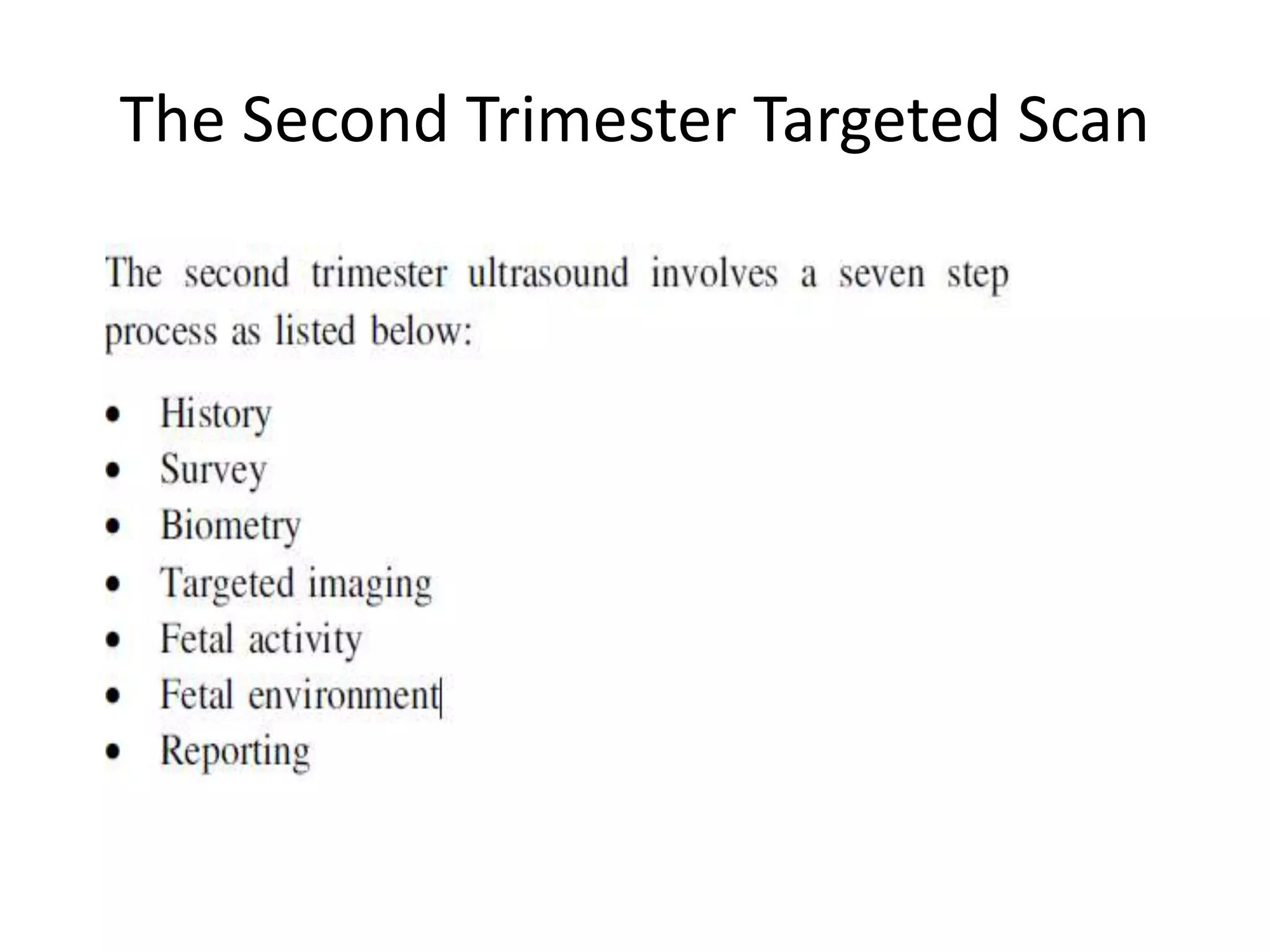
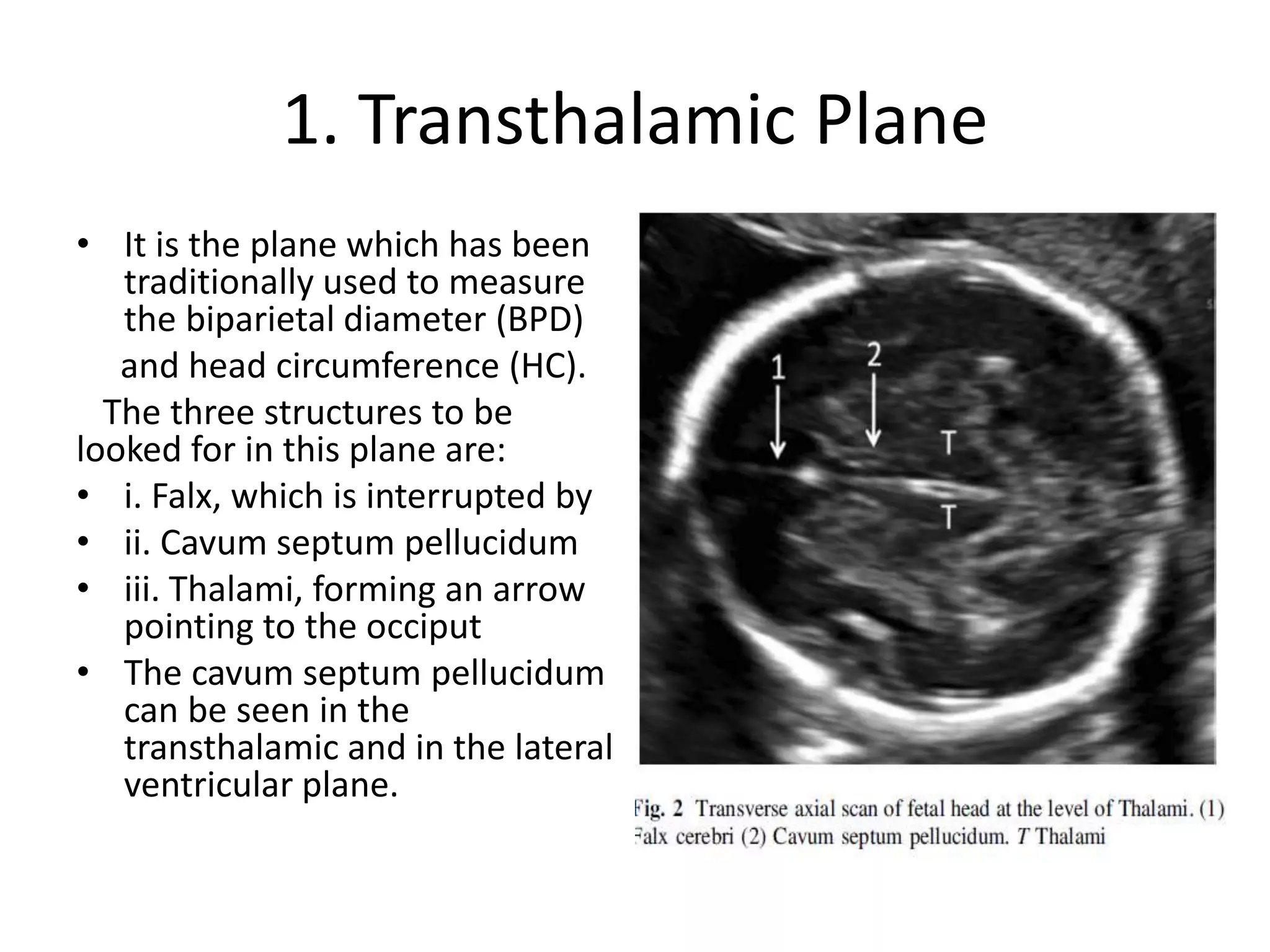
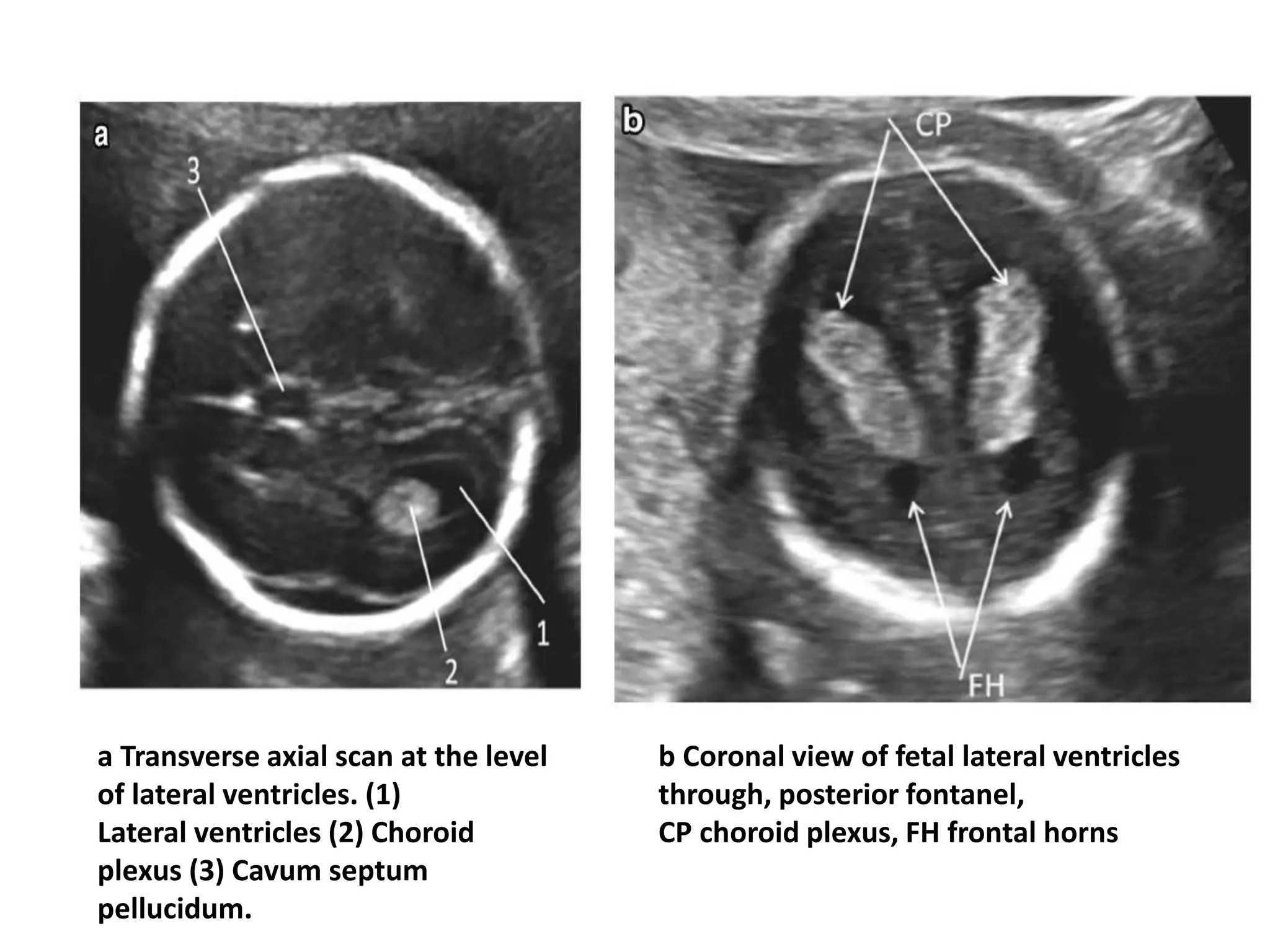
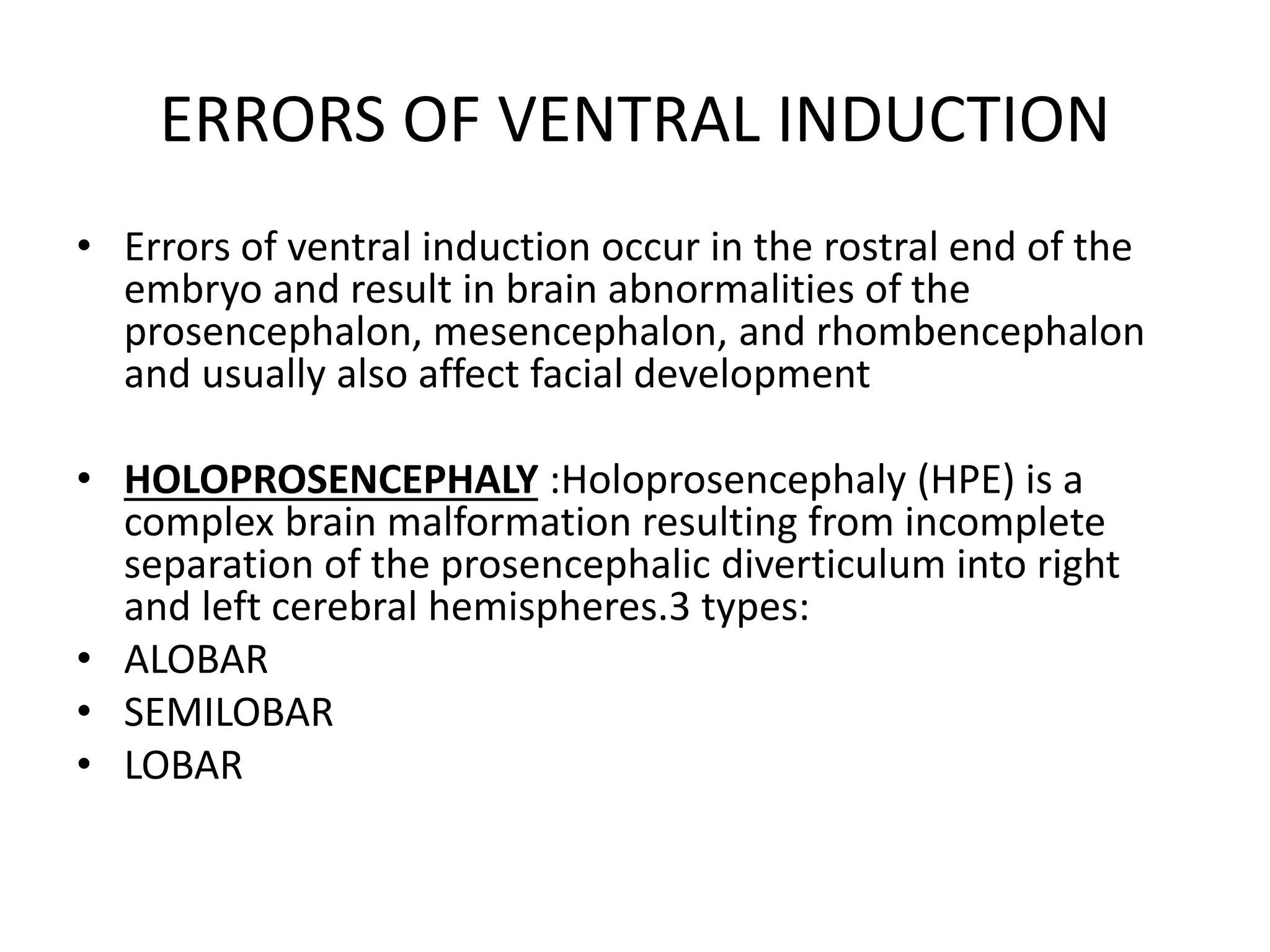
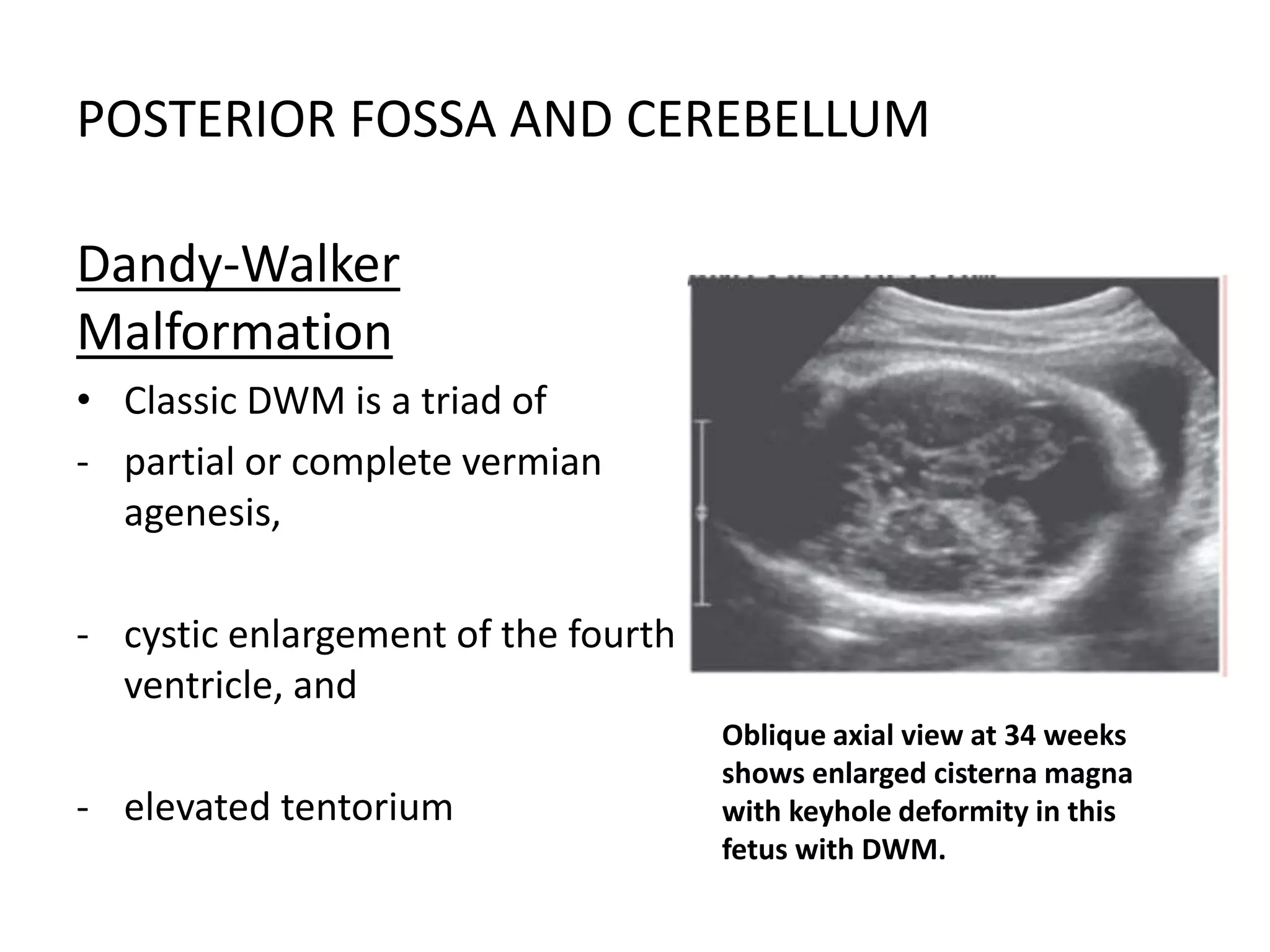
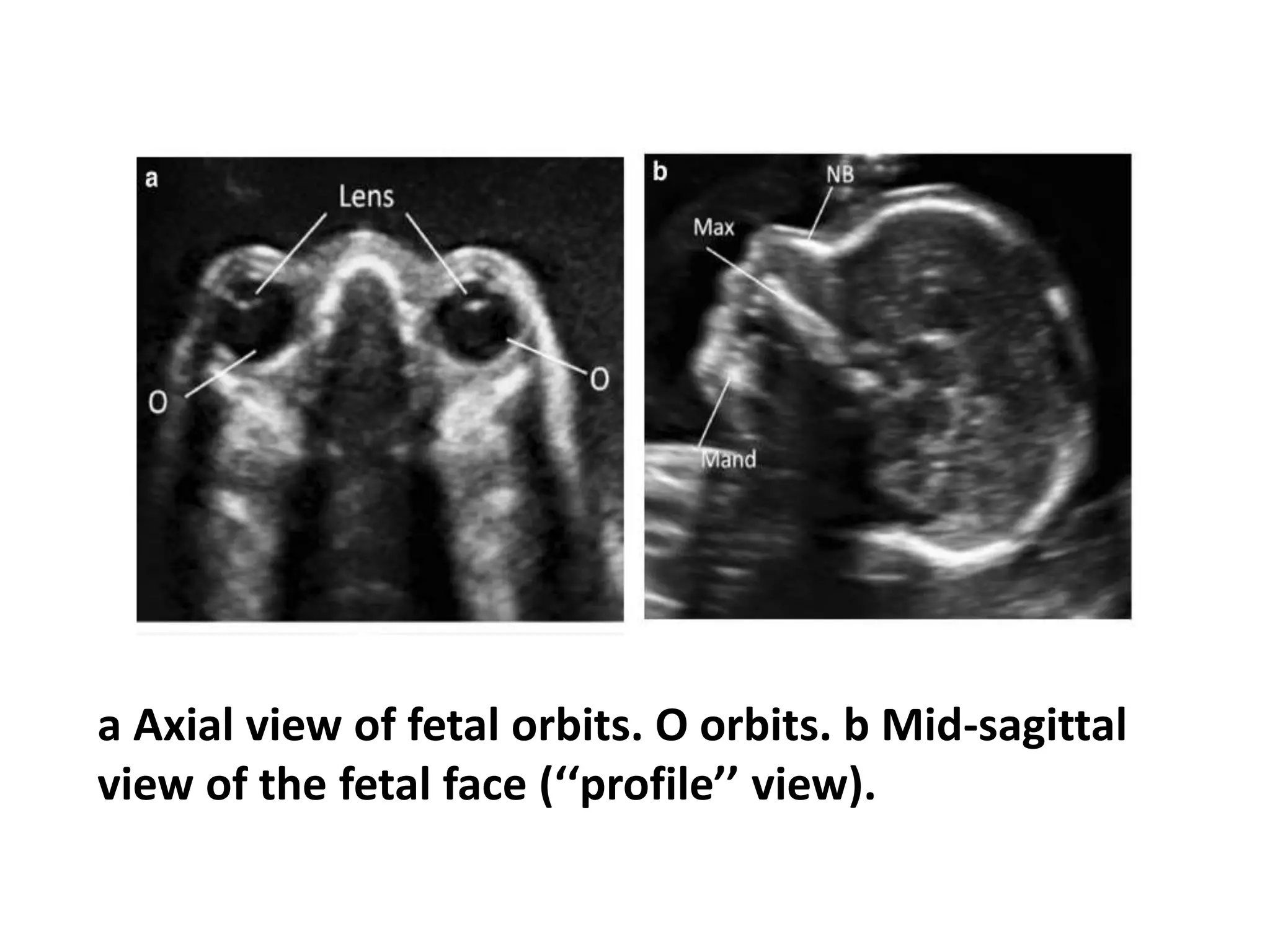
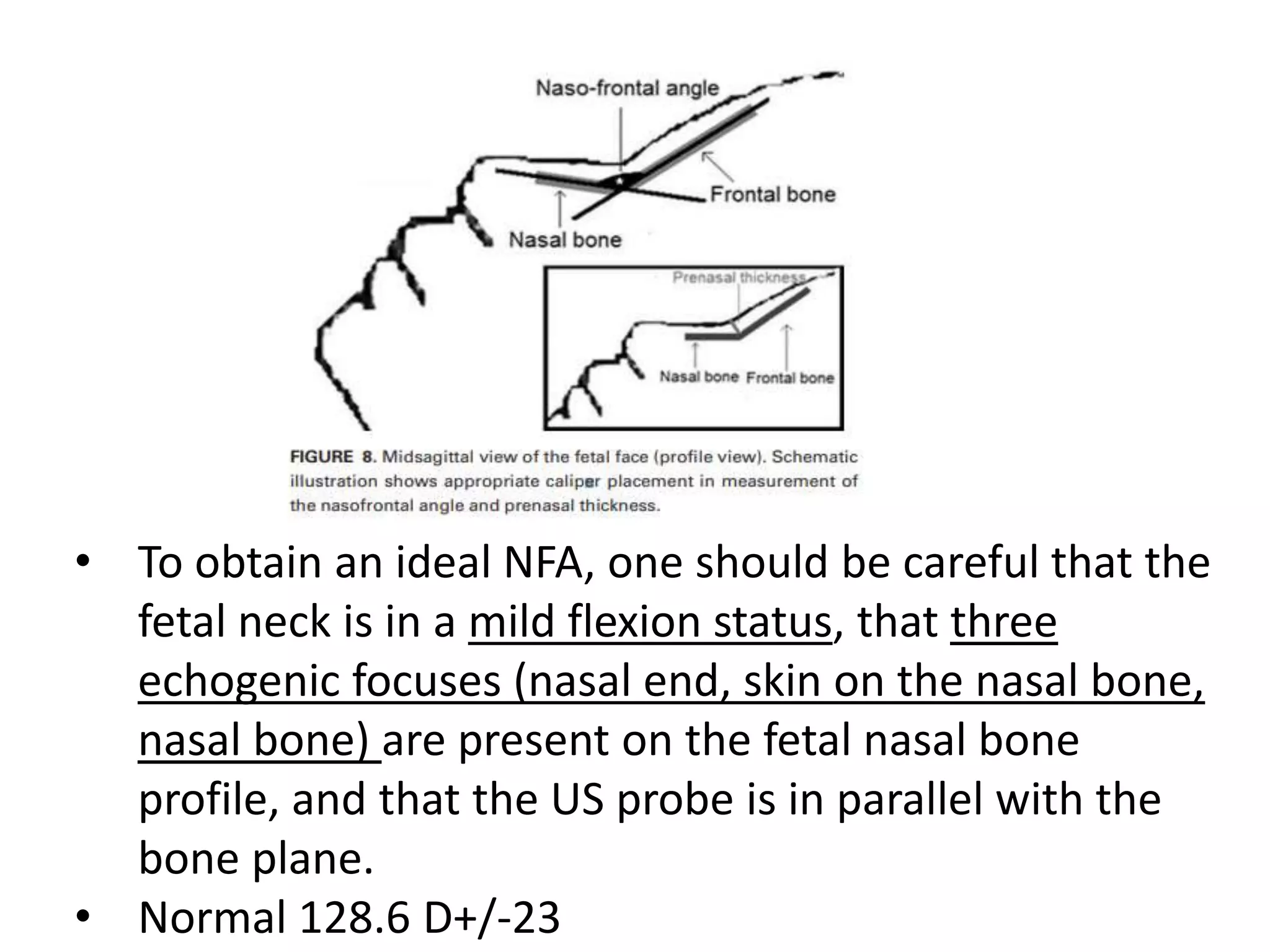
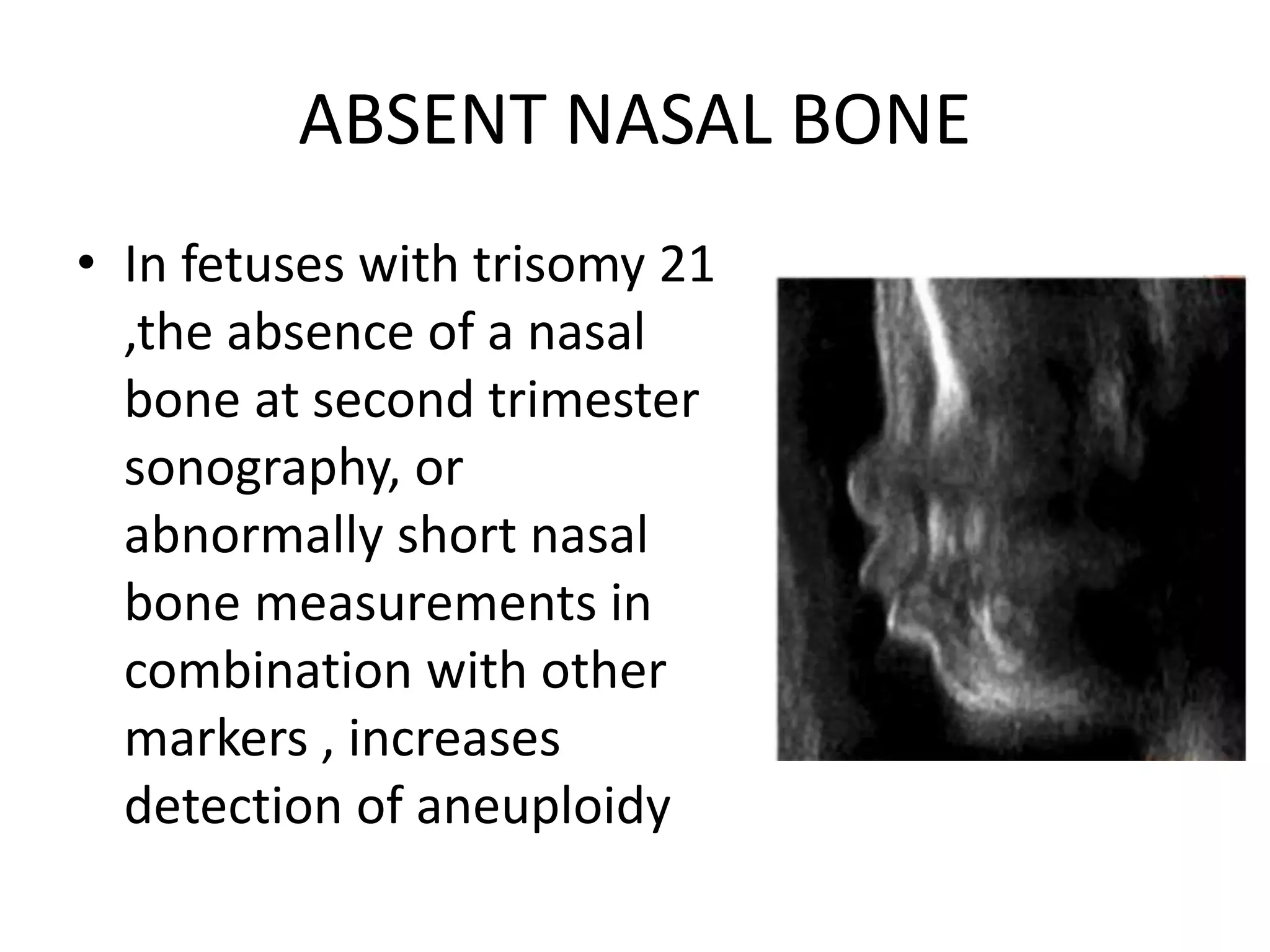
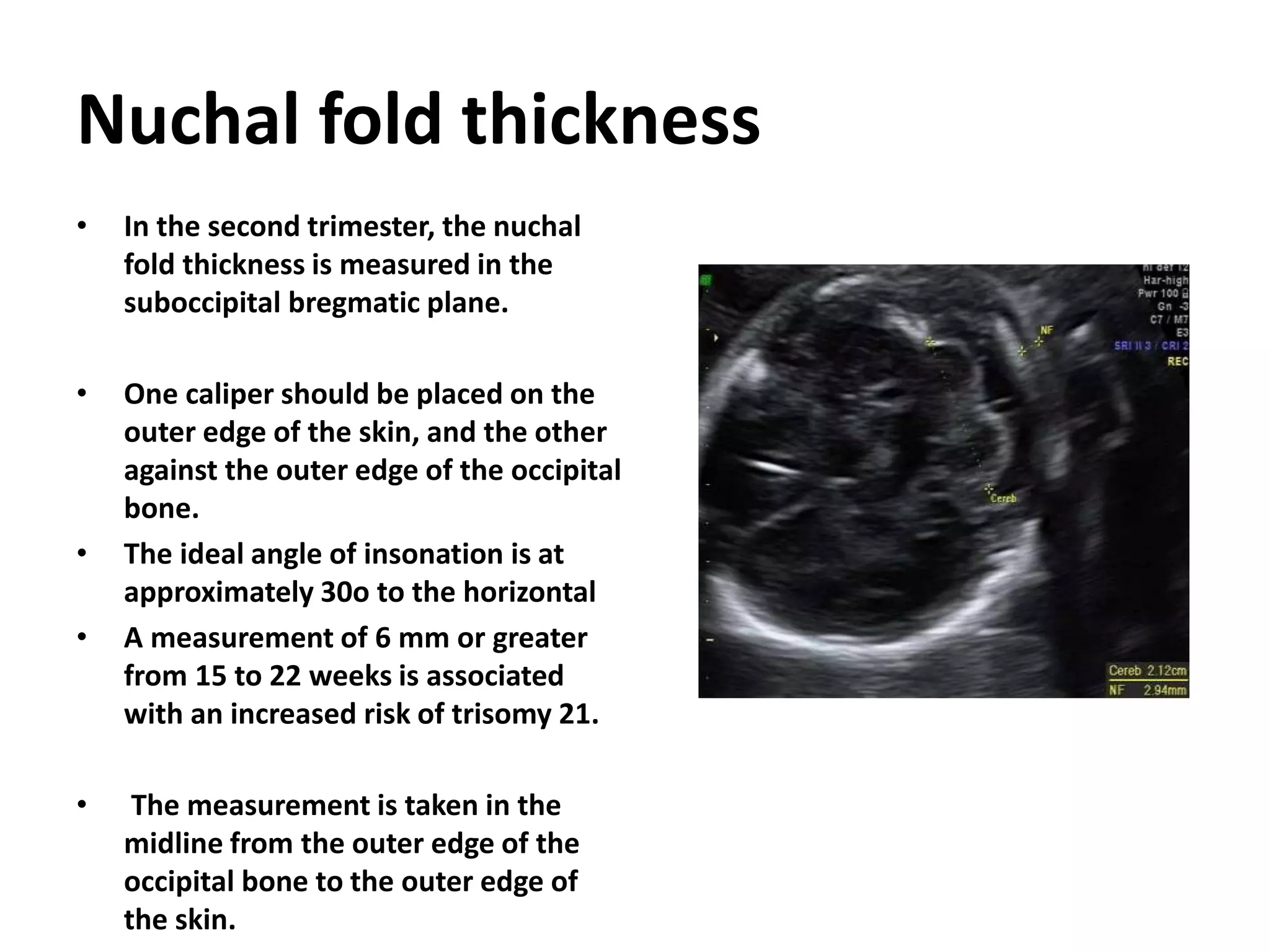
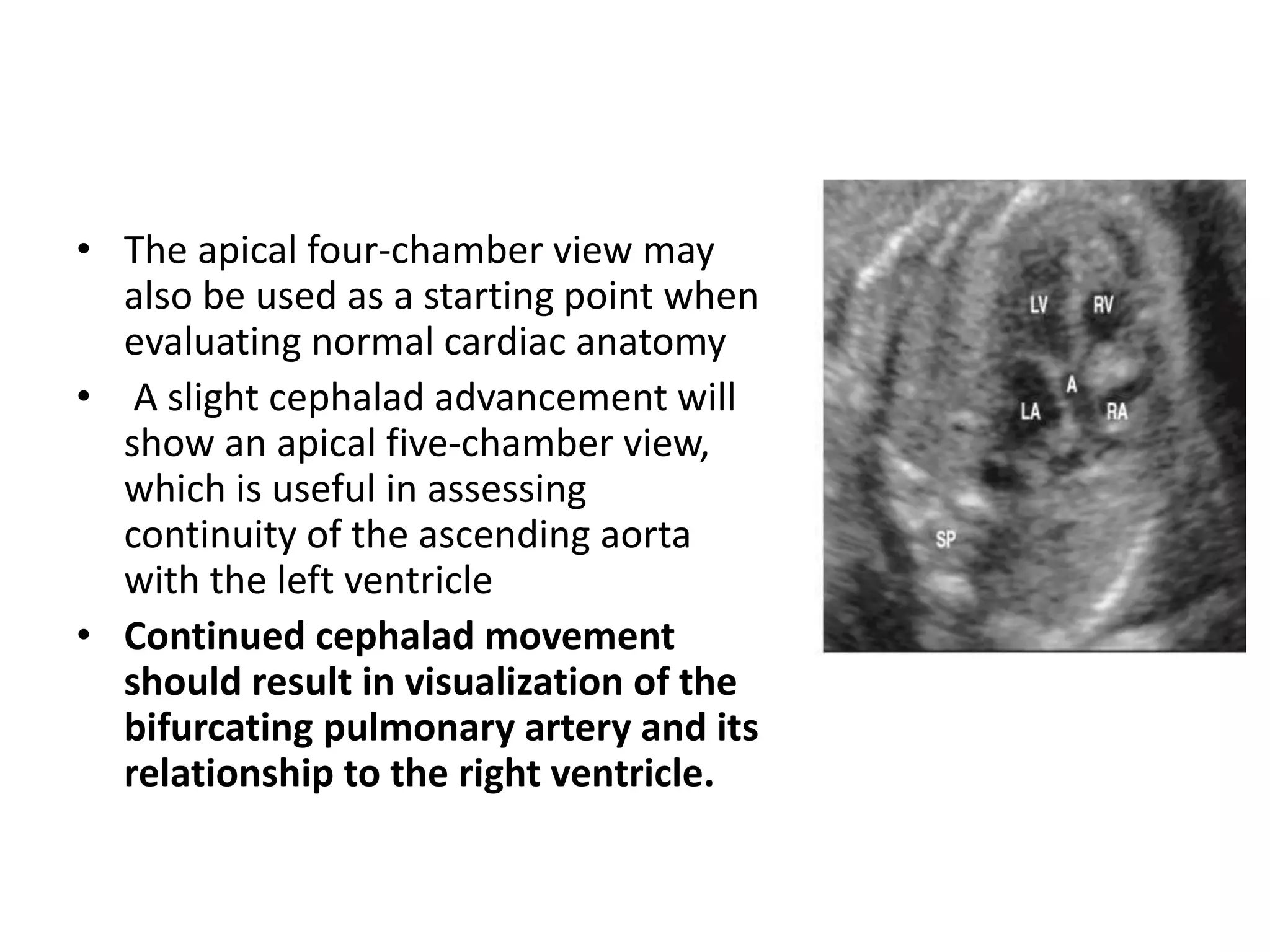
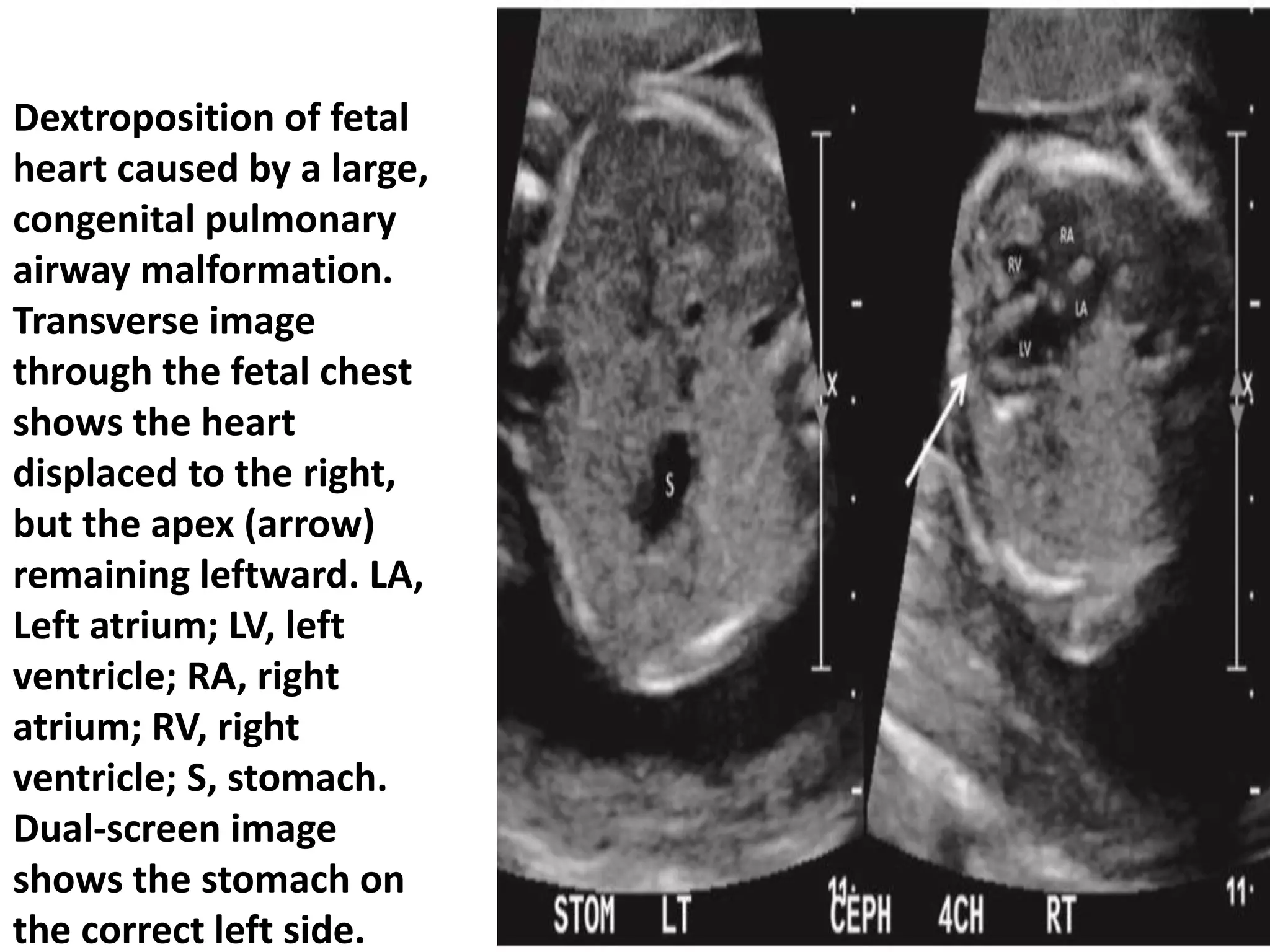
This document describes the fetal anomaly scan, also known as the second trimester targeted scan, which is performed between 18-22 weeks gestation to evaluate fetal anatomy and detect any anomalies. It outlines the "Rule of Three" systematic scanning method to thoroughly examine the head, face, and other structures. Specific anatomical planes and landmarks are identified for different areas, along with common variations and abnormalities that may be seen. The objectives are to determine normalcy, identify severe abnormalities, and raise suspicion of potential issues warranting further evaluation.
























































































![Phone No: 4477923/4476152
SECOND TRIMESTER ANOMALY SCAN REPORT
(Reporting template by Nepal Radiologist Association)
Patient Name: Ms Age/Sex: yrs/ Female
Patient/USG No:0 Contact number:
Accompanying person: Relation
Referring doctor: KMCTH (Gynae/Obs) Date of examination:2078-01-19
Measurements:
Parameter Measurement ( in mm) Corresponding GA (W+D)
BPD mm weeks days
HC mm weeks days
AC mm weeks days
FL mm weeks days
EDD
Estimated foetal weight (EFW): gms
Parameters:
Foetal heart rate (FHR): beats per minute (Regular)
Presentation: Cephalic/Breech/Transverse
Liquor volume Adequate
Placenta: Fundal/Anterior/Posterior
Upper /Lower
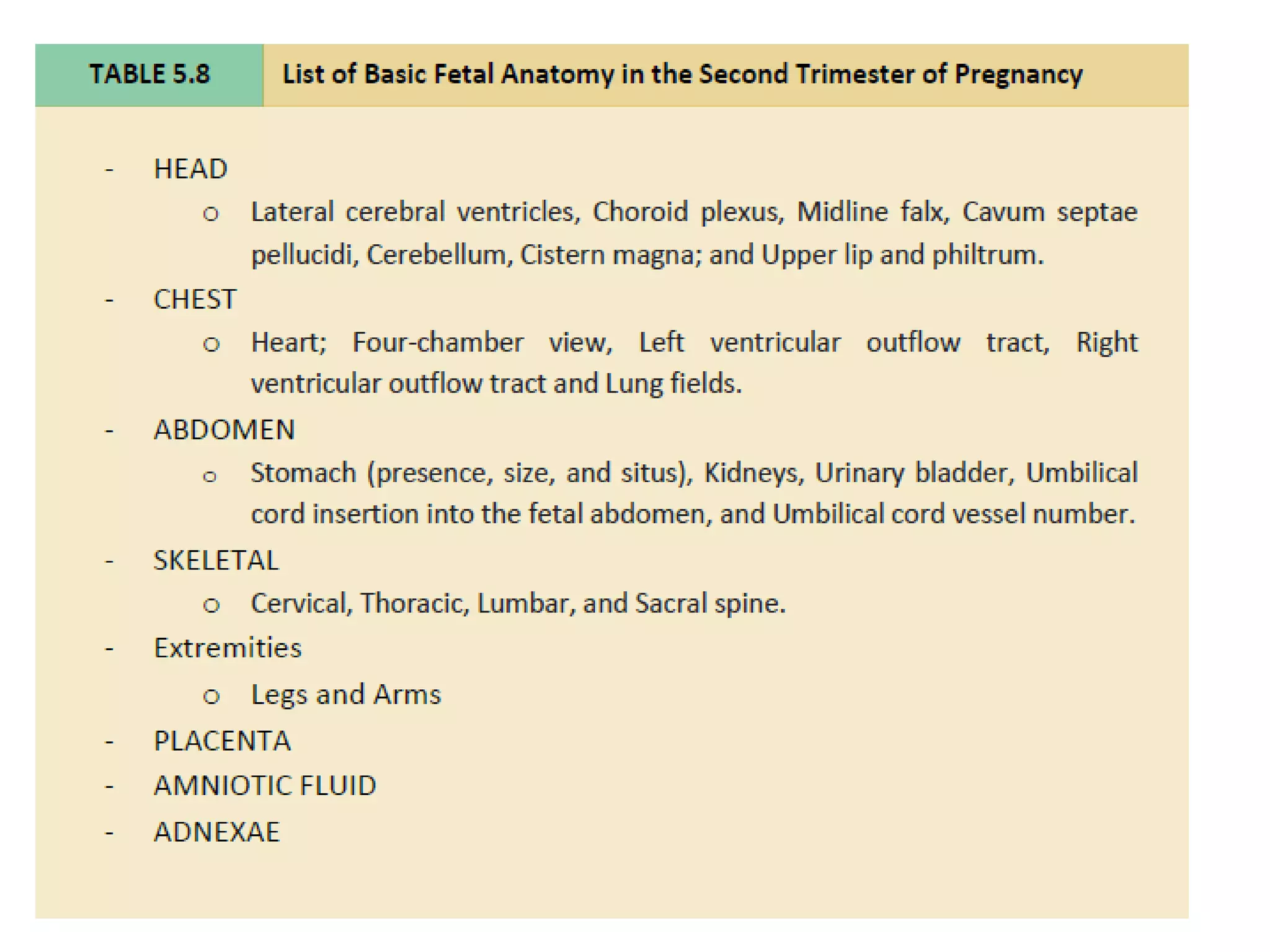
Structural study of foetal anomaly: [N: Normal, Abn: Abnormal, NA: Not assessed/limited study, Prn: image printed]
Head Neck/Thorax Abdomen
Shape N Shape N Stomach N
Cavum septi
pellucidi
N No masses N Bowel N
Midline falx N Heart Kidneys N
Thalami N Activity N Urinary bladder N
Lateral
ventricle
N Size N Abdominal cord
insertion
N
Cerebellum N Axis N 3 vessel cord N
Cisterna
magna
N Four
chamber
view
N Spine N
Face Limbs
Upper lip N Both arms and
hands
N
Nose N Both legs and feet N
Orbits N
Median
profile
N
Additional comments:……………………………………………………………………………………………………………………….
Final conclusion:
Single live intrauterine foetus of weeks days of gestation and gms by BPD/HC/FL.
____________
Dr. Jatati Shahi
MBBS, MD
Radiologist
Note: This scan does not include screening for cardiac anomaly.
Each & every congenital anomaly cannot be detected by 2D ultrasound.](https://image.slidesharecdn.com/fetalanomalyscan-210514145055/75/Fetal-anomaly-scan-121-2048.jpg)

