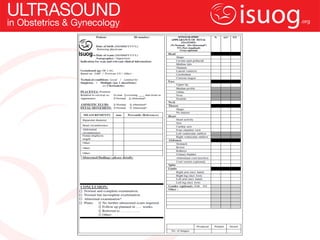
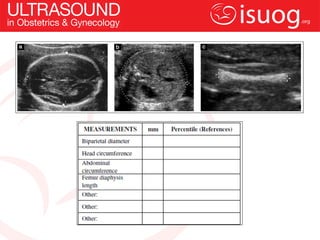
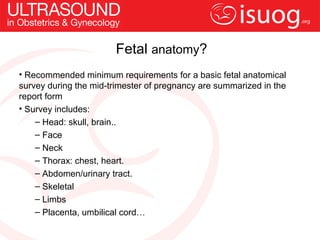
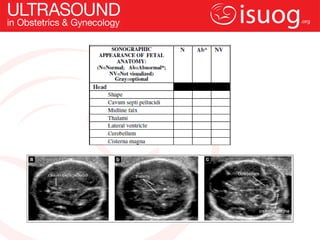
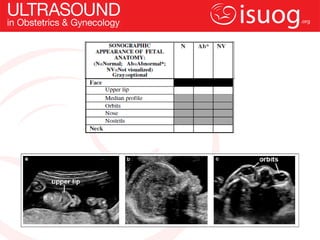
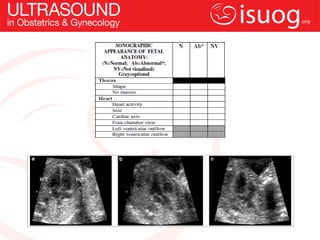
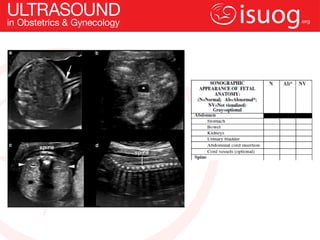
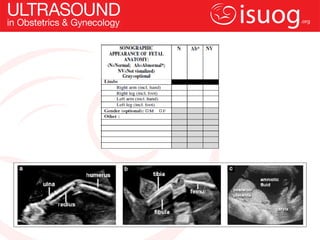
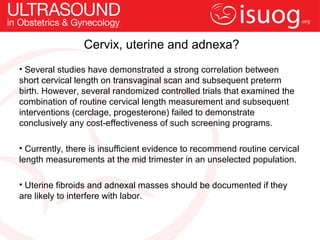
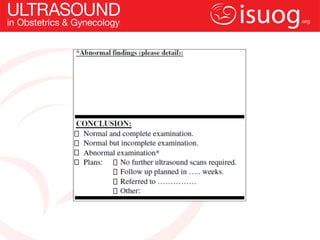
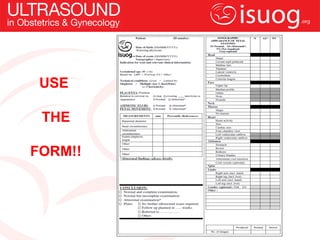
This document provides guidelines for performing mid-trimester fetal ultrasound scans from the International Society of Ultrasound in Obstetrics and Gynecology (ISUOG). It discusses the purpose of the scans, who should perform them, necessary equipment, what should be included in reports, safety considerations, assessing fetal well-being and biometry, examining fetal anatomy, and evaluating the cervix, uterus and adnexa. The guidelines emphasize providing accurate information to optimize care, while minimizing risk, and include a sample reporting form.