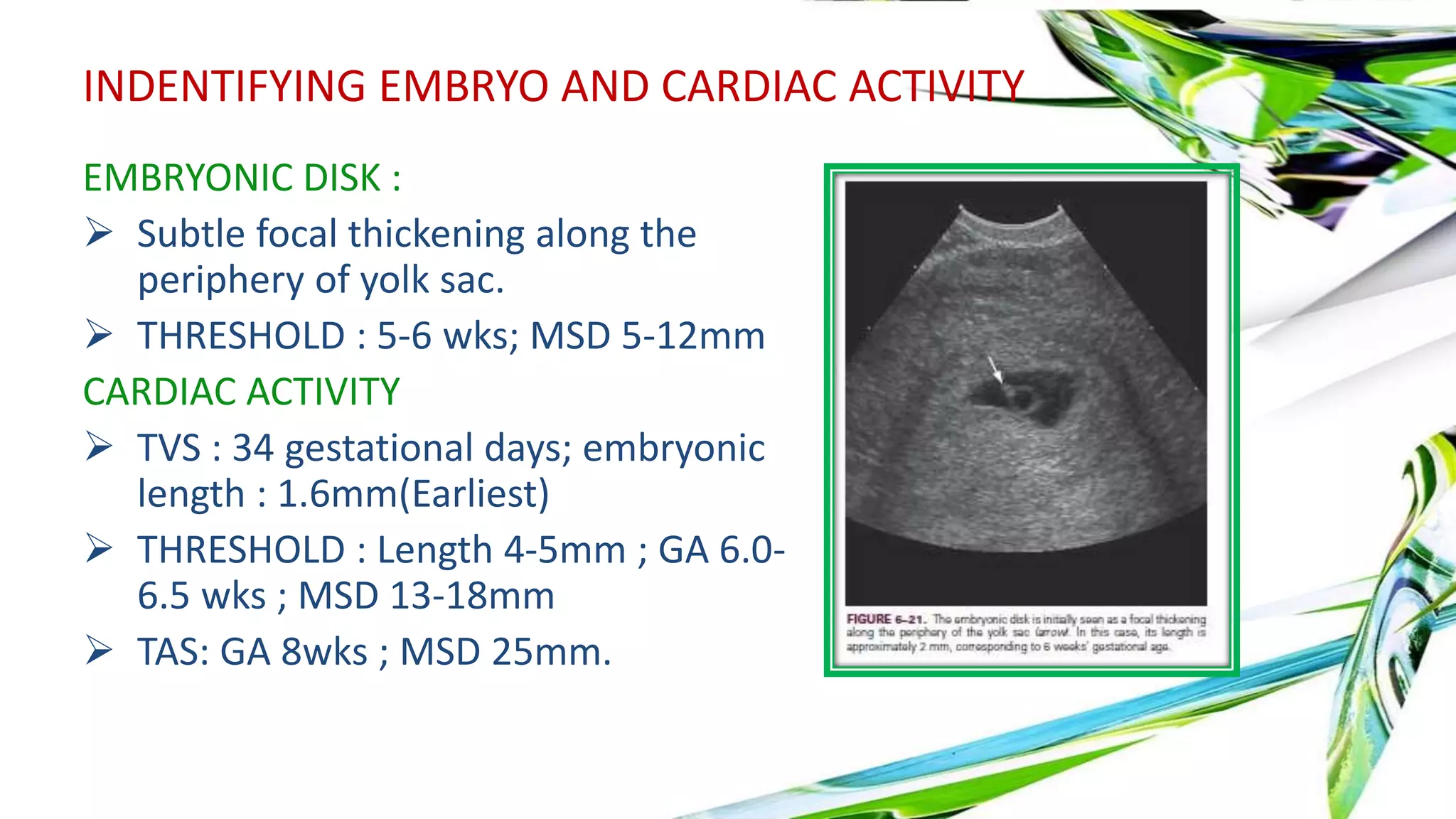
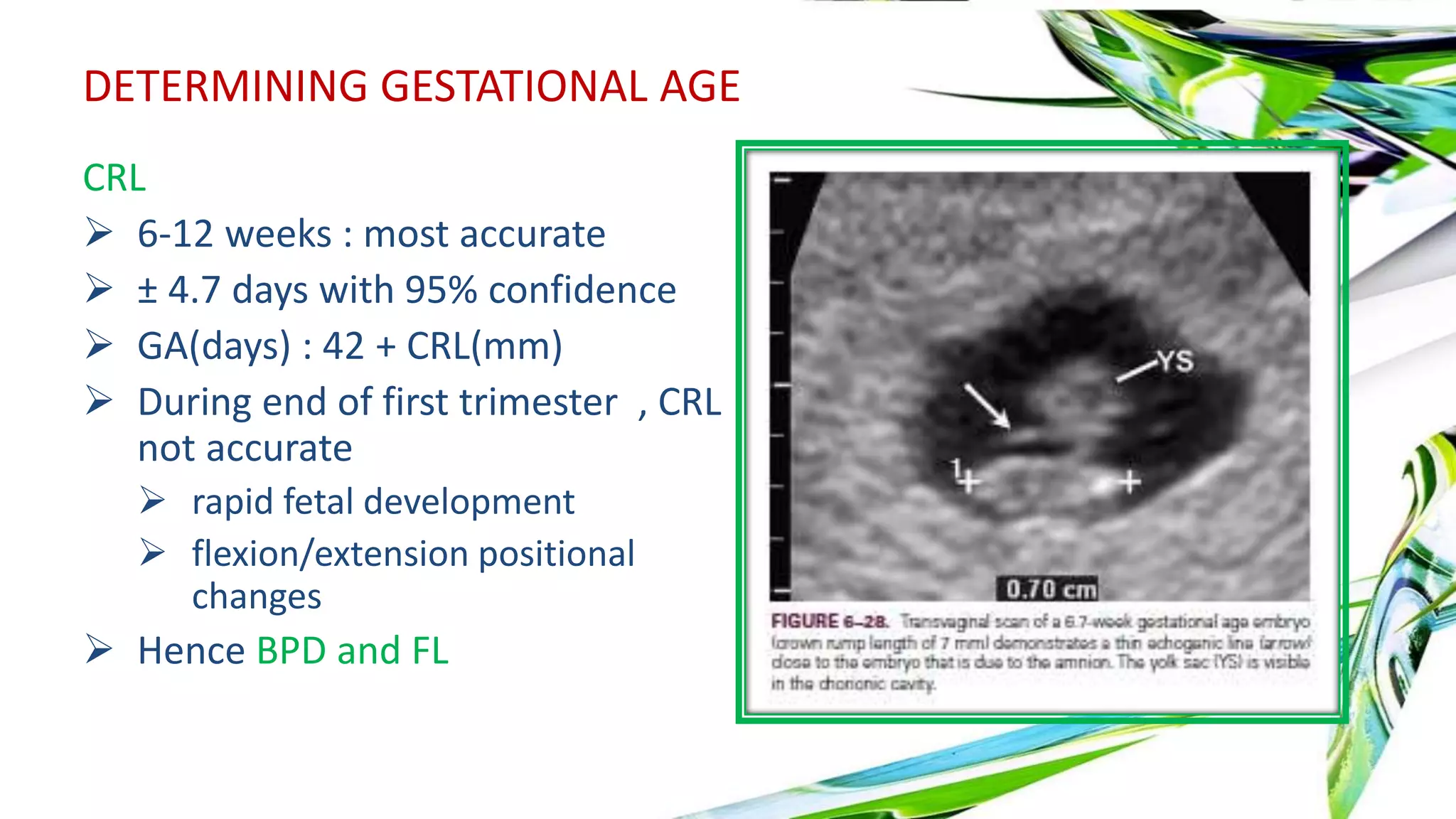
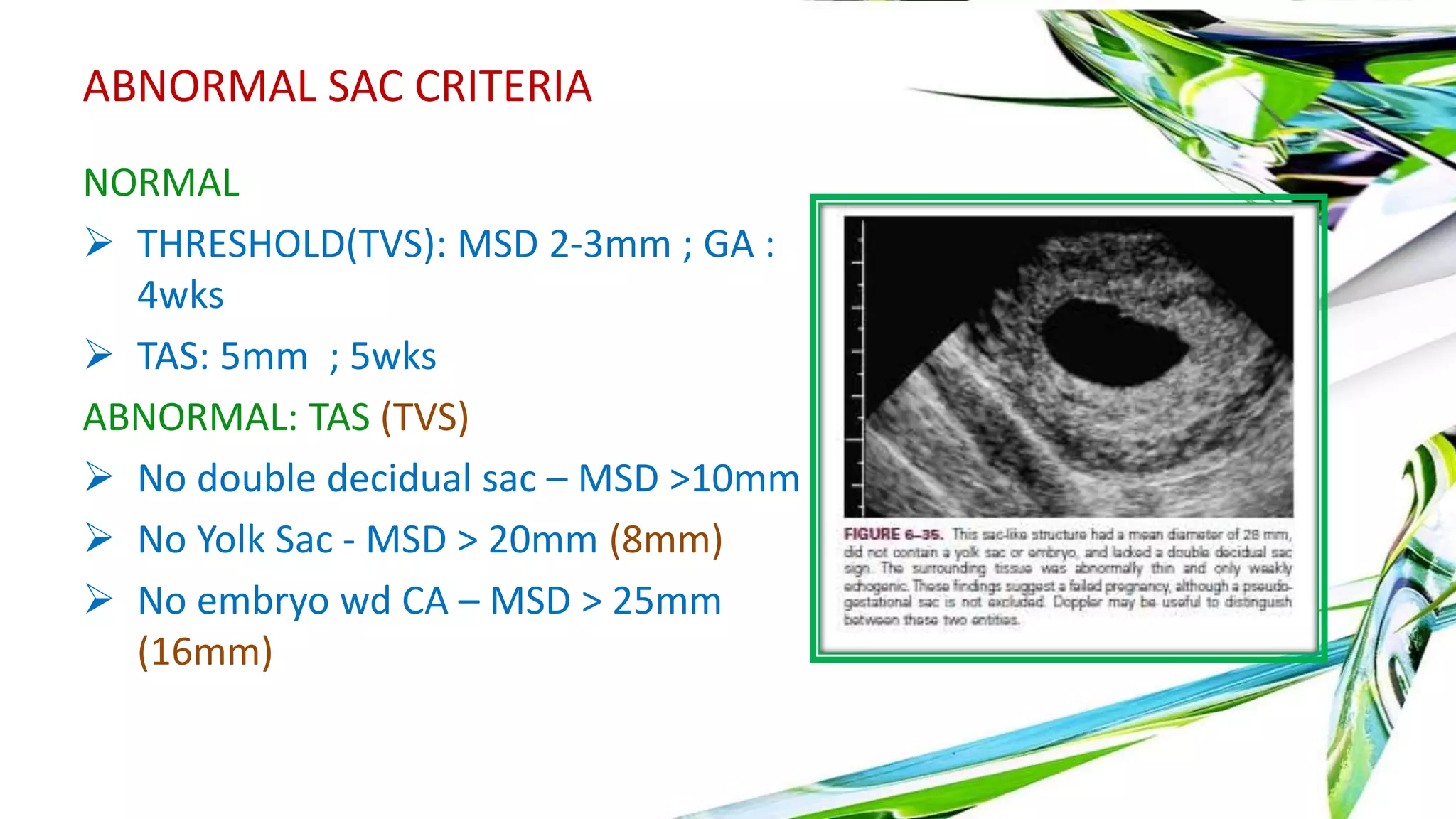
Ultrasound is useful in the first trimester for evaluating bleeding, pain, gestational sac location and development. A gestational sac is normally visible by 4 weeks ultrasound. The yolk sac appears by 5 weeks and the embryo with cardiac activity by 6 weeks. Abnormal findings include lack of growth, irregular sac shape, large yolk sac size. Doppler can assess blood flow. Ectopic pregnancies can be detected by visualizing an embryo outside the uterus combined with serum hCG levels. Multiple pregnancies are determined by membrane thickness and number of yolk sacs.