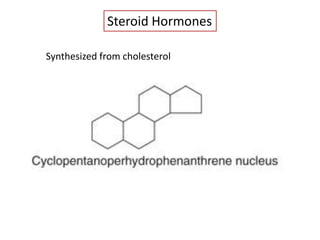
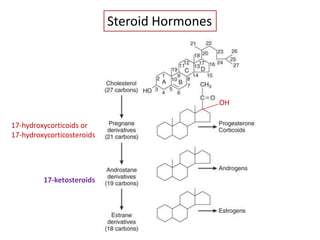
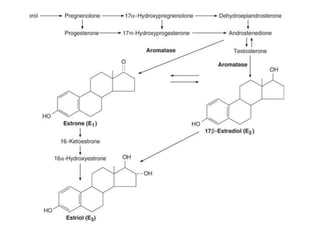
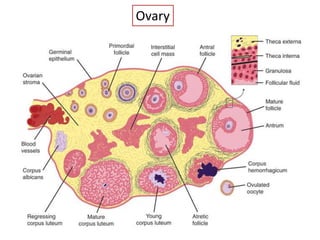
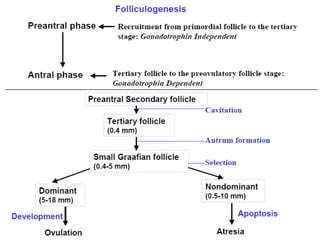
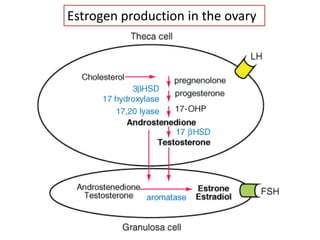
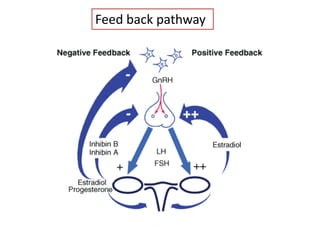
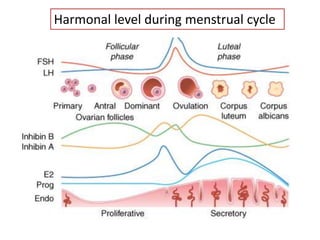
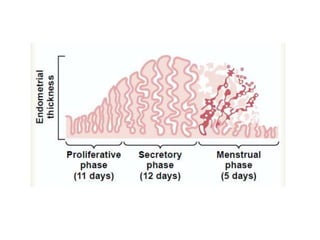
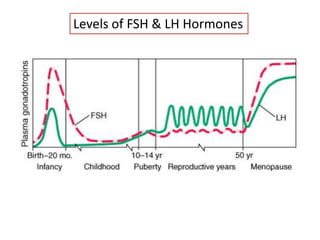
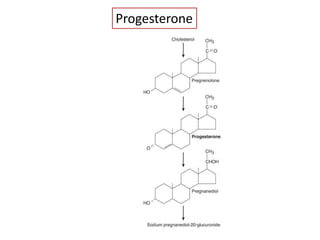
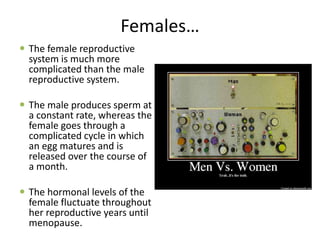
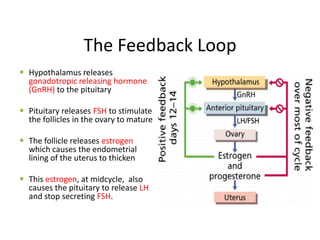
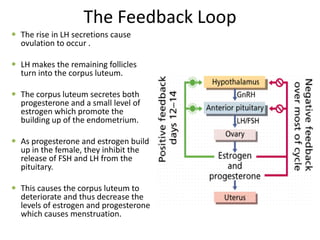
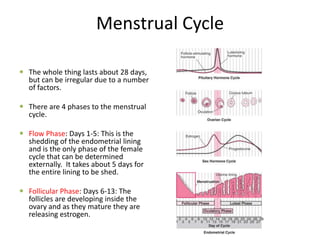
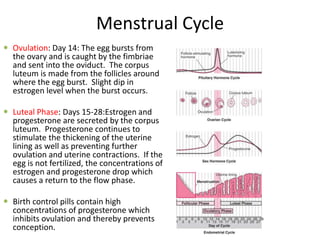
The document summarizes female hormone synthesis and function. It discusses how the ovary orchestrates oocyte development and release while also producing hormones like estrogen and progesterone. These hormones regulate the menstrual cycle and prepare the uterus for potential pregnancy. The cycle involves fluctuations in hormone levels that influence the development and shedding of the uterine lining over approximately 28 days until menopause ends the female reproductive years.