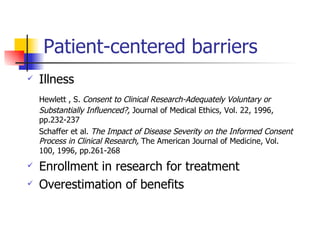
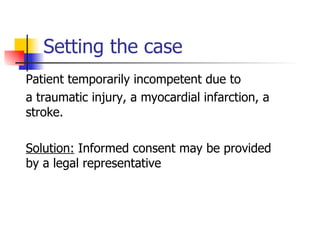
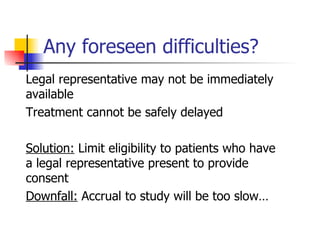
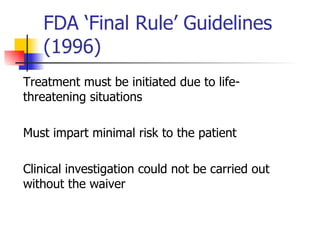
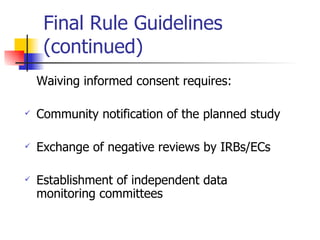
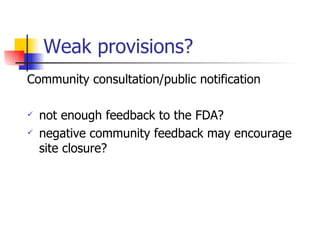
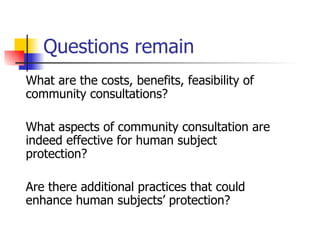
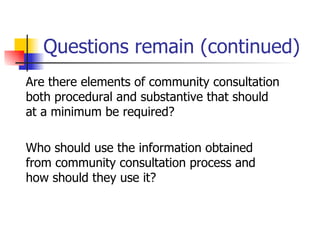
This document discusses challenges around obtaining informed consent from vulnerable populations in medical research. It explores two case studies: research in emergency settings where patients may be temporarily incompetent, and research with cancer patients where illness can impact competency. For both cases, it examines difficulties around ensuring understanding while obtaining consent, and proposes alternatives like deferred consent or waiving consent with additional protections. Throughout, it emphasizes finding the right balance between individual autonomy, beneficence, and justice when conducting research with vulnerable groups.