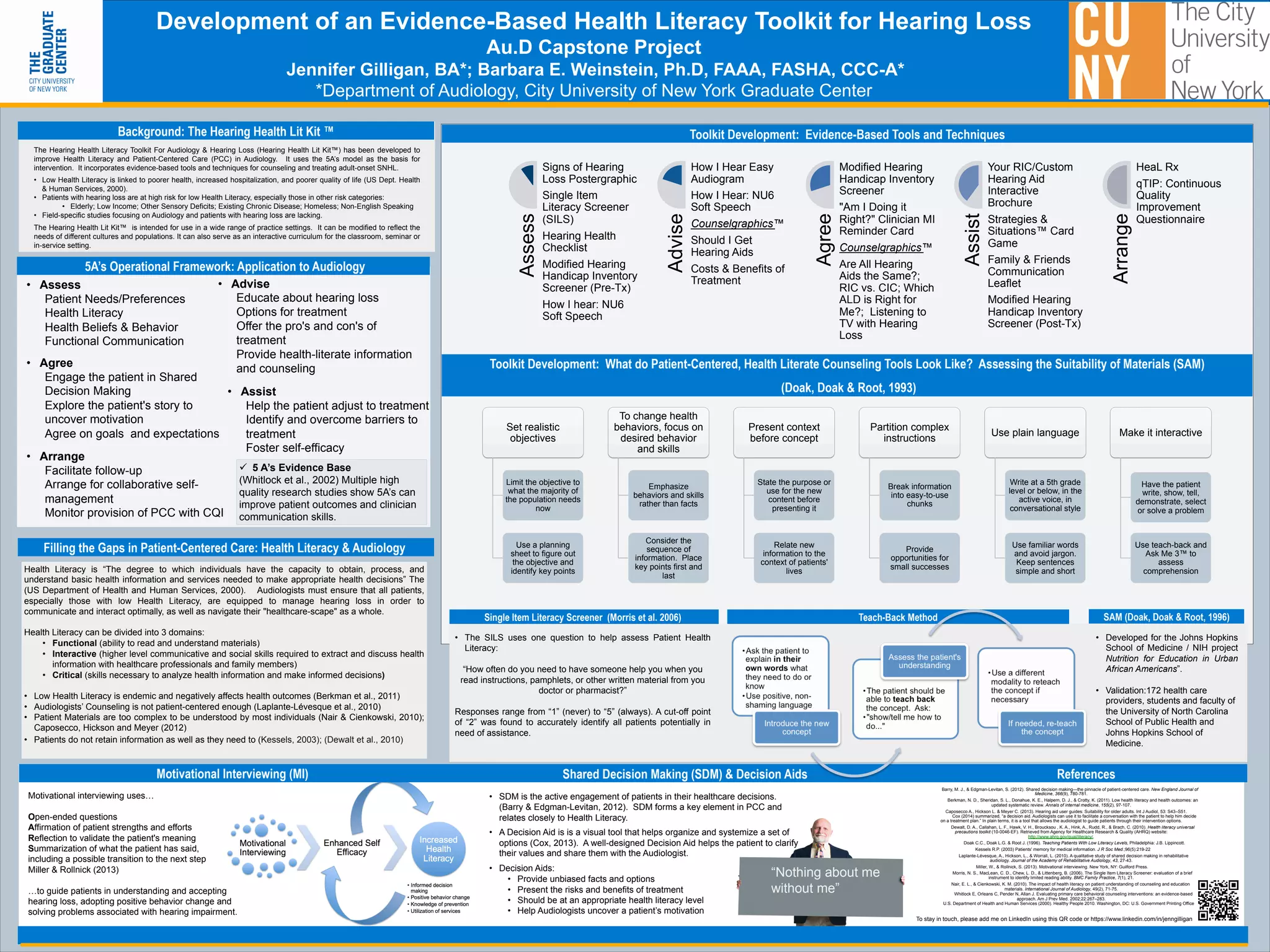
This document describes the development of an evidence-based health literacy toolkit for hearing loss. It discusses low health literacy rates and issues with existing patient materials and counseling in audiology. The toolkit, called the Hearing Health Literacy Toolkit, uses the 5 A's model (Assess, Advise, Agree, Assist, Arrange) as a framework. It incorporates tools and techniques grounded in health literacy principles, motivational interviewing, shared decision making, and patient-centered care to improve how audiologists educate and treat patients with hearing loss. The goal is to help patients better understand and manage their condition.