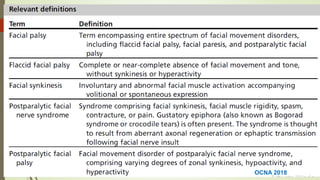
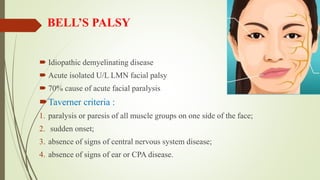
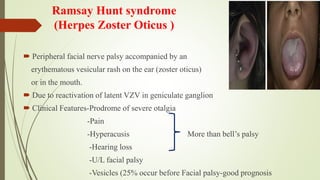
The document provides information on the facial nerve (CN VII) including its anatomy, branches, segments, development and disorders. Some key points:
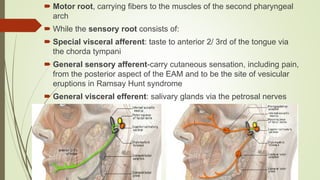
- The facial nerve has motor and sensory components and contains fibers for facial expression, taste, and lacrimal/salivary glands.
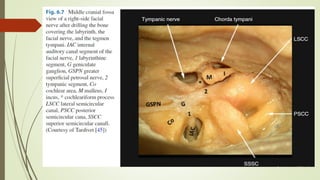
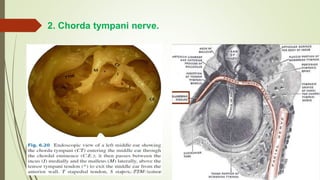
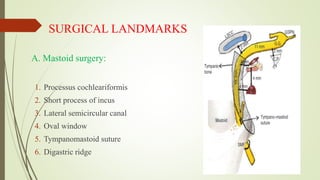
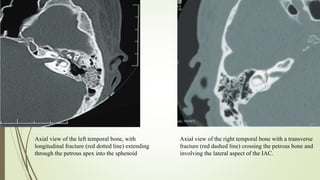
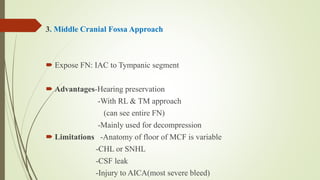
- It exits the skull via the stylomastoid foramen and has segments within the skull, internal auditory canal, middle ear and mastoid.
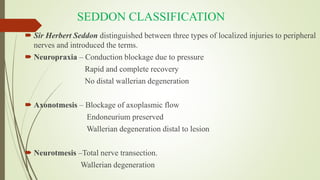
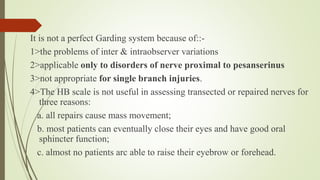
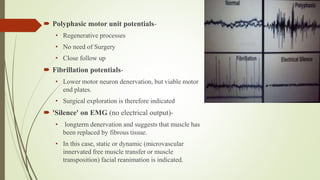
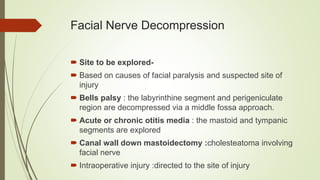
- Injuries are classified using Seddon or Sunderland systems based on the level of nerve disruption.
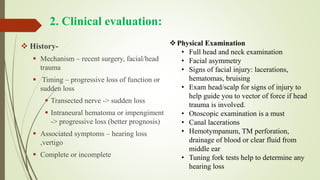
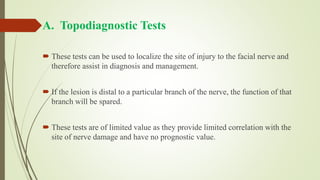
- Evaluation includes tests of lacrimal, stapedius, taste and salivary functions to localize the lesion. Electrodiagnostic tests assess prognosis