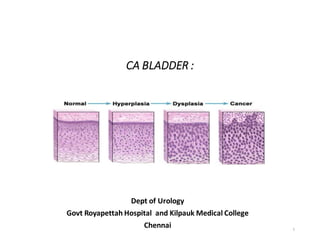
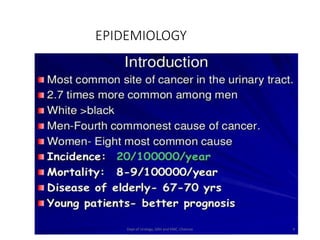
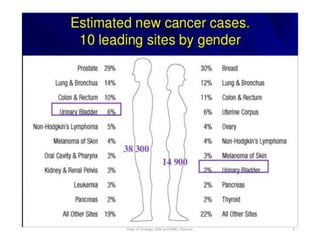
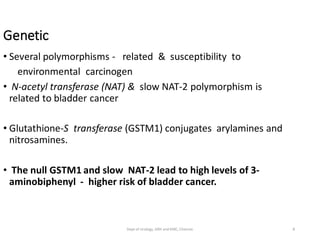
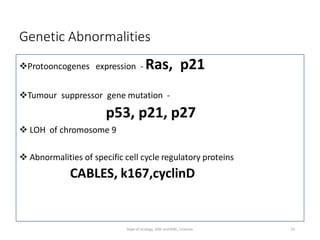
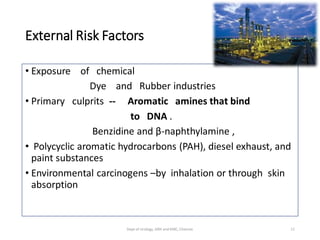
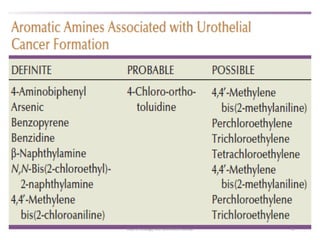
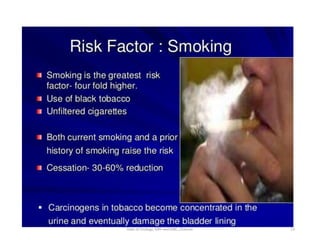
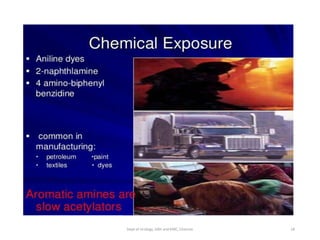
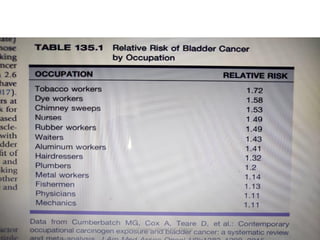
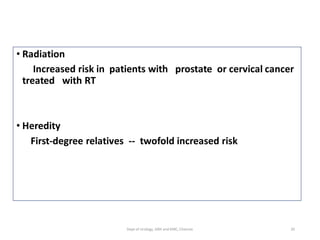
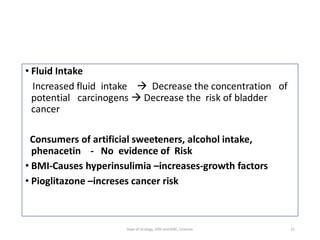
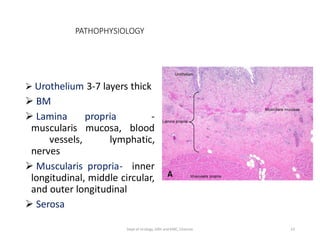
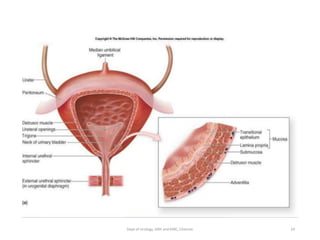
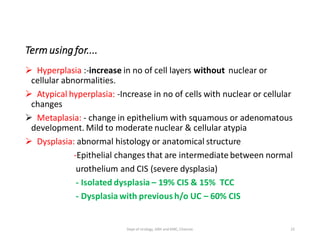
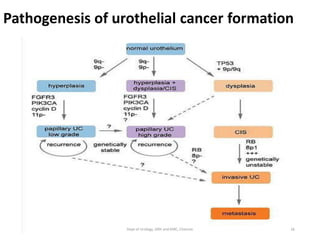
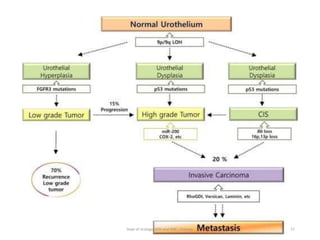
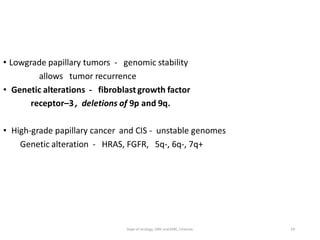
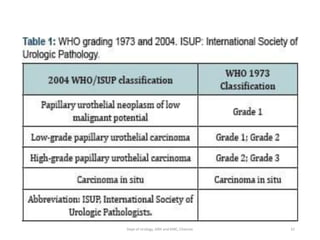
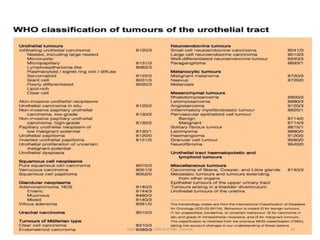
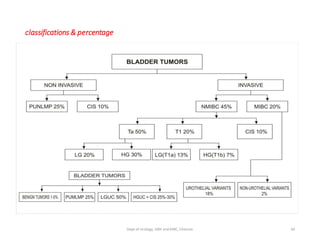
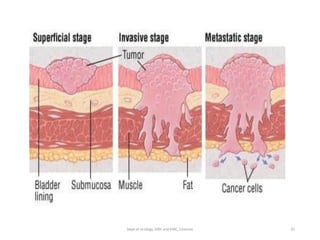
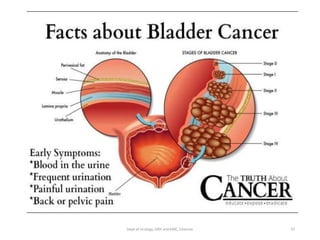
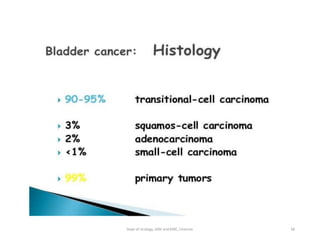
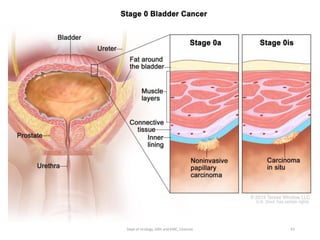
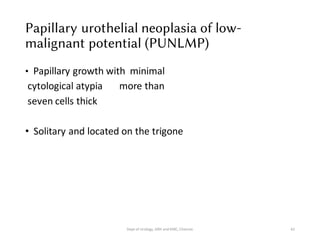
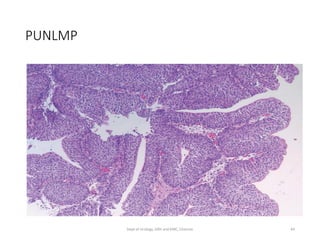
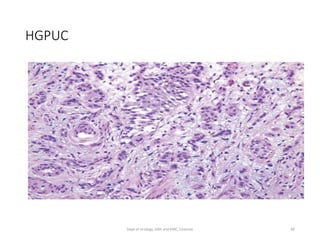
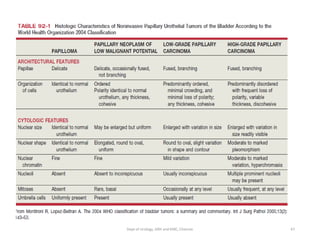
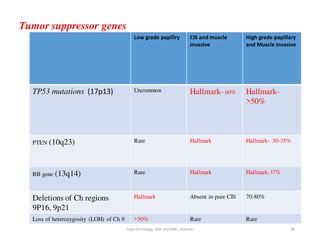
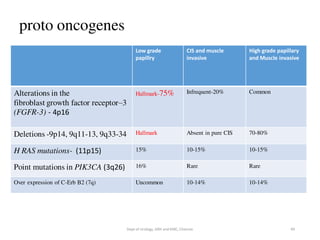
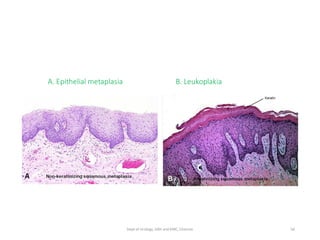
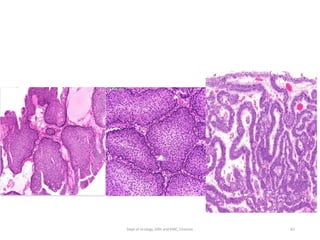
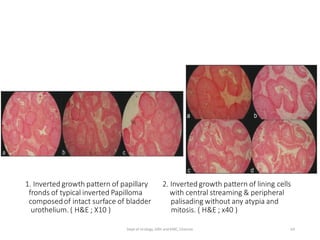
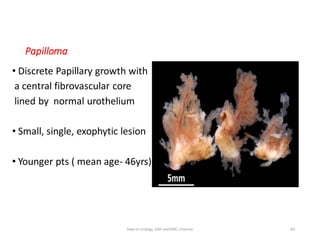
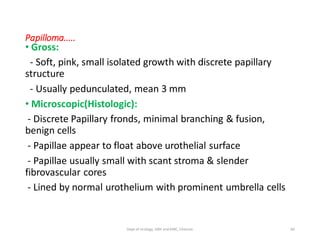
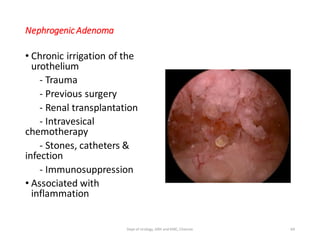
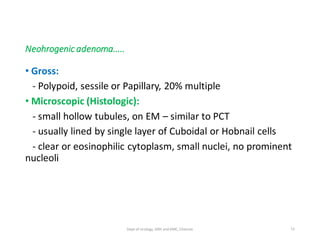
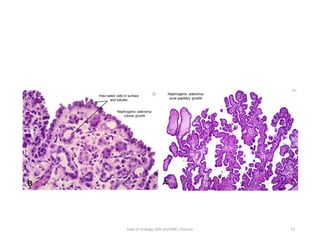
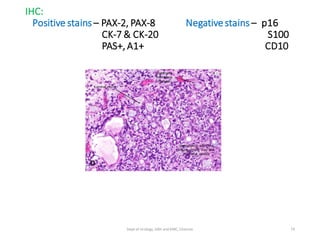
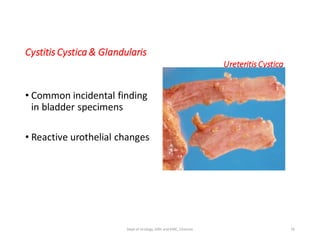
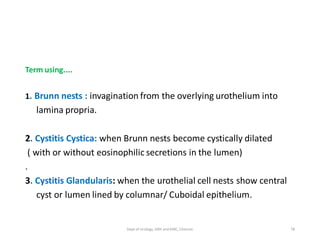
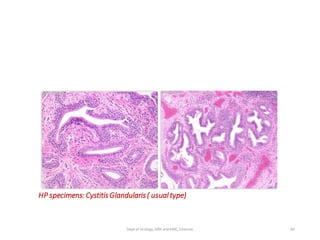
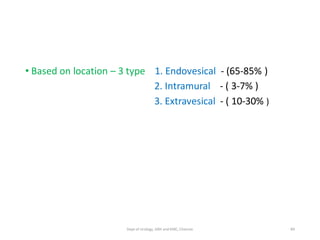
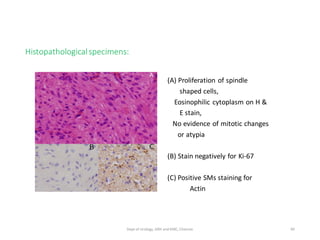
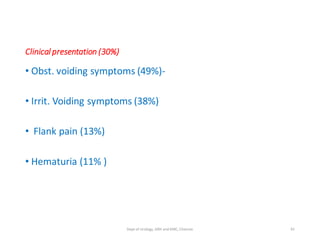
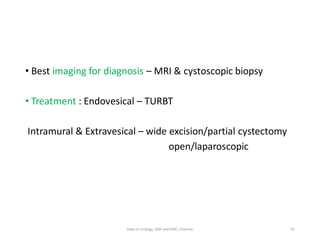
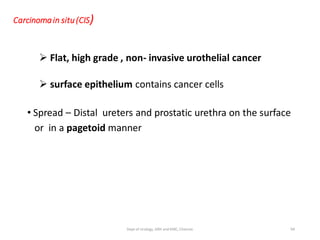
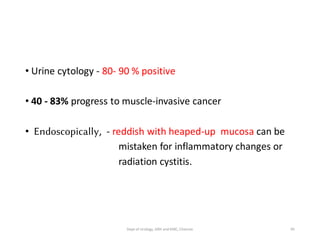
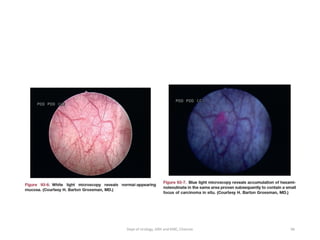
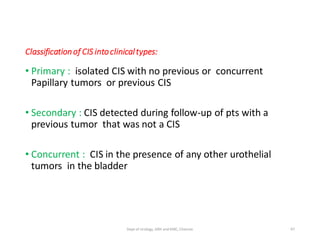
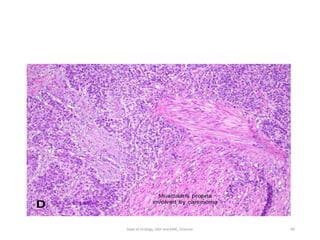
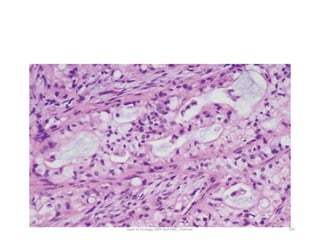
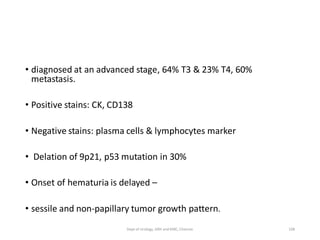
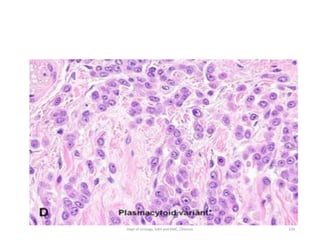
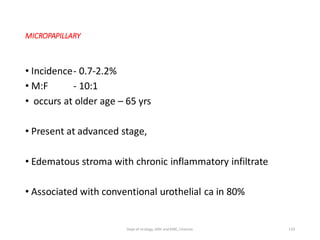
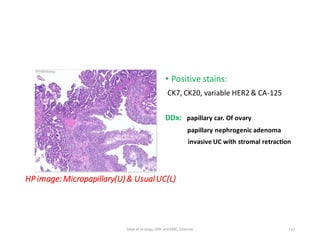
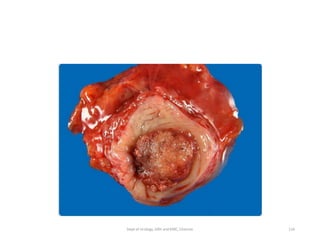
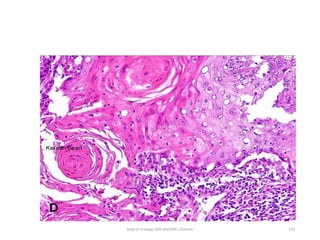
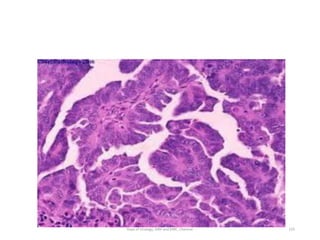
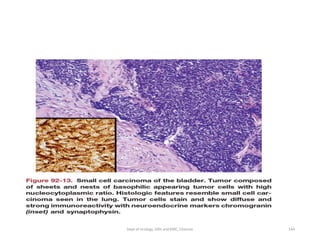
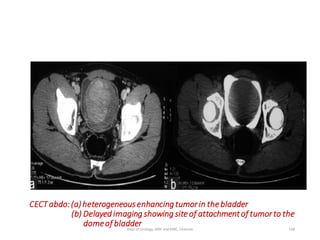
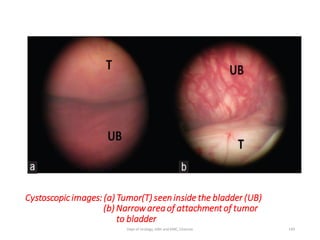
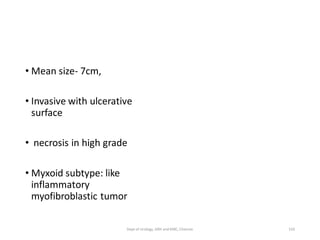
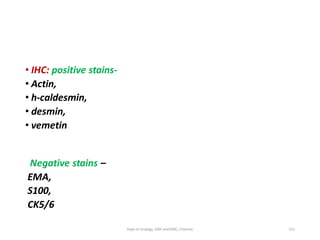
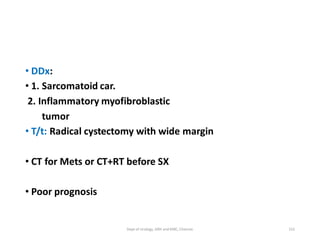
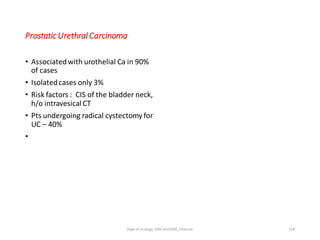
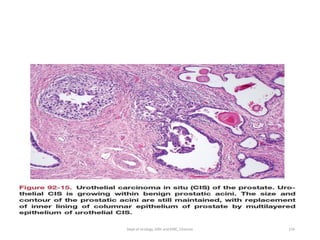
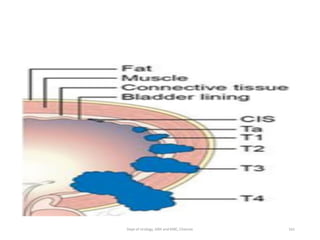
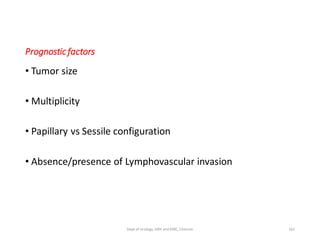
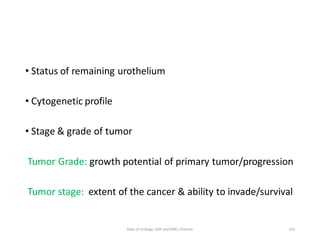
This document discusses bladder cancer and provides information on epidemiology, etiology, pathophysiology, classification, clinical features, and histopathology of benign and malignant bladder tumors. It is from the Department of Urology at Govt Royapettah Hospital and Kilpauk Medical College in Chennai, India. The document lists the moderators and their academic titles. It then covers topics such as the higher prevalence of bladder cancer in men compared to women, risk factors including smoking and occupational exposures, genetic factors, pathogenesis, WHO and other classification systems, clinical features of non-muscle invasive and muscle invasive bladder cancers, histopathology of benign lesions and different grades of bladder tumors.