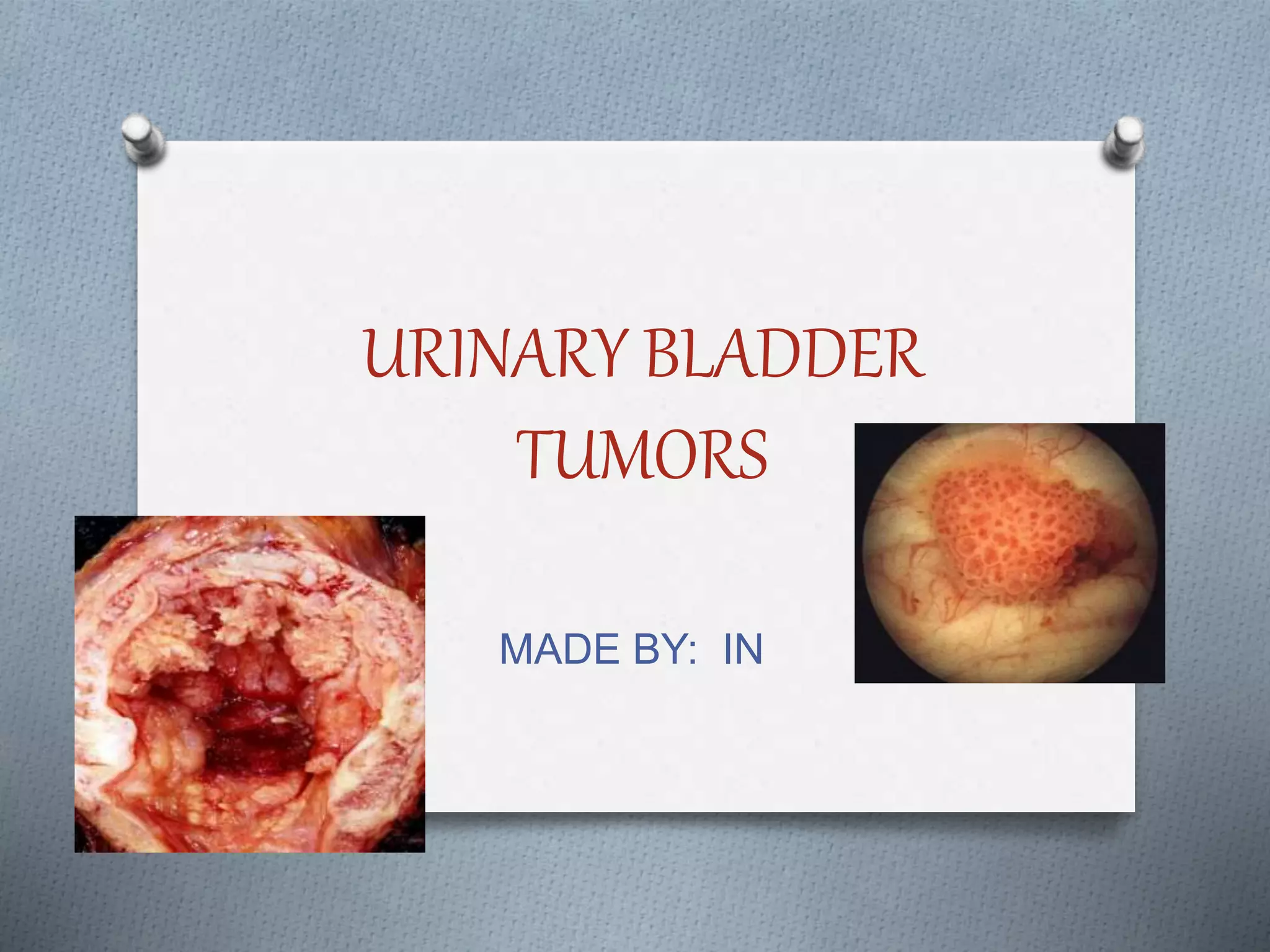
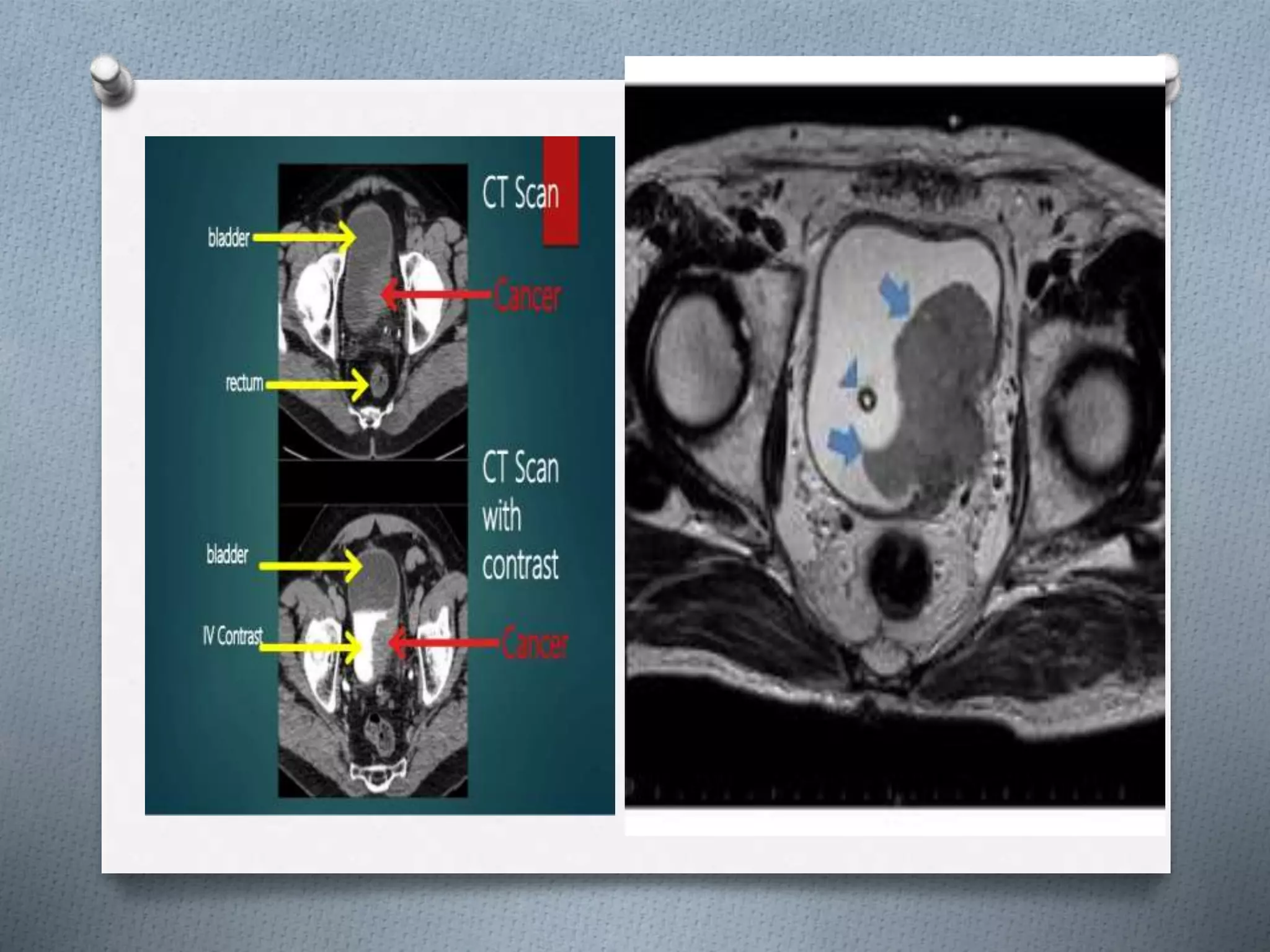
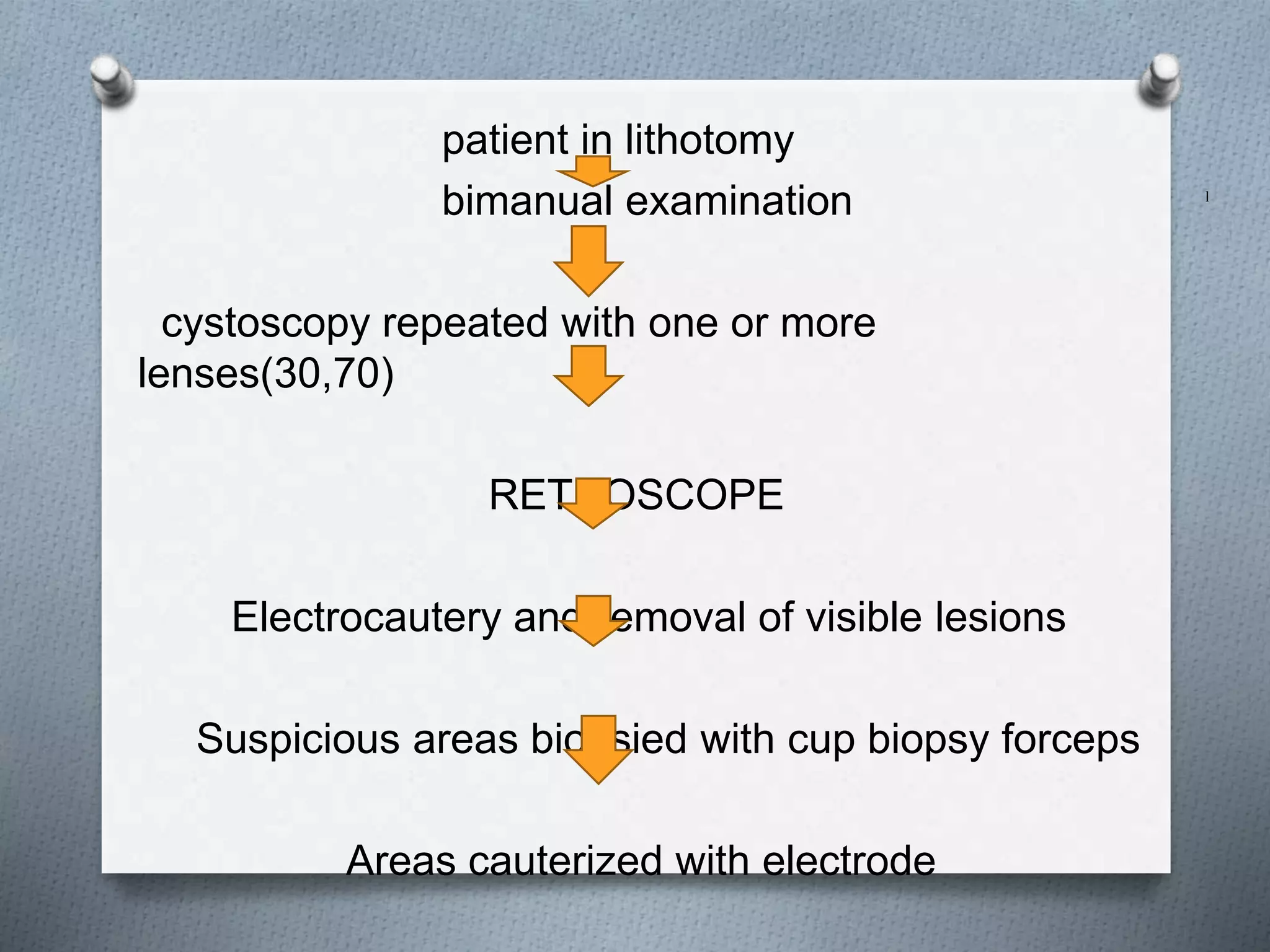
The urinary bladder is a hollow muscular organ that temporarily stores urine before expulsion. It has an apex, fundus, body, neck, and urethra. Blood supply comes from branches of the internal iliac arteries. Lymphatic drainage occurs to internal and external iliac lymph nodes. The bladder wall has layers of transitional epithelium, lamina propria, and muscularis propria. Bladder cancer is the second most common genitourinary cancer, with smoking being the main risk factor. Symptoms include hematuria. Diagnosis involves cystoscopy, biopsy, and imaging to stage the tumor. Treatment depends on tumor stage and grade but may include transurethral resection and intravesical