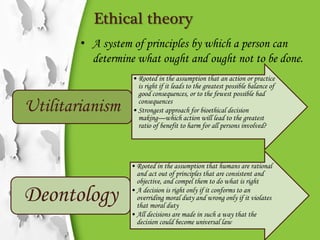
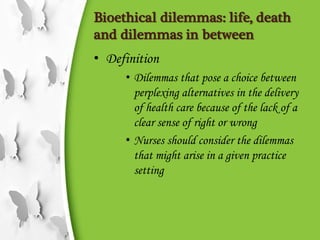
Bioethical issues in nursing presents key concepts in bioethics including definitions of bioethics, importance of bioethics in healthcare, and common bioethical situations nurses may encounter. Some key points discussed are:
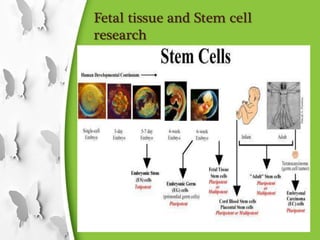
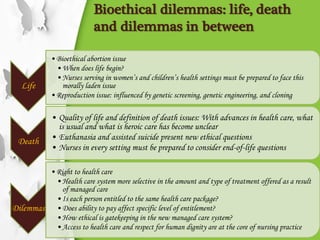
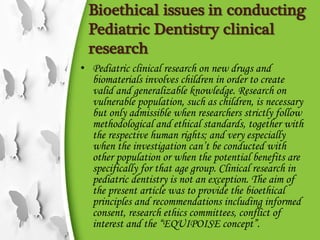
- Bioethics studies ethical implications of new biological discoveries and advances in fields like genetics and drug research.
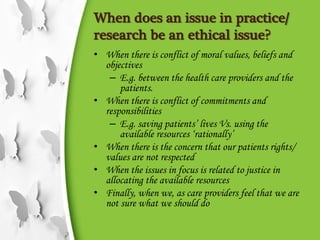
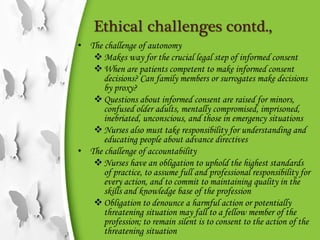
- Understanding bioethics is important for nurses due to ever-changing medical policies, patient rights, and new clinical issues.
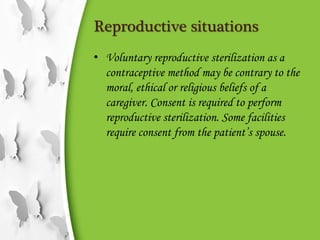
- Common bioethical issues addressed include reproductive situations like sterilization and abortion, human experimentation, and dealing with infectious diseases like HIV/AIDS.
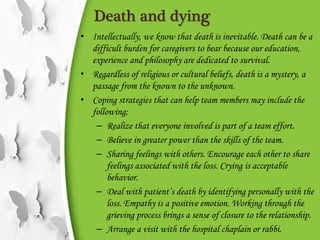
- Nurses must consider ethical issues around quality of life, end-of-life care, organ