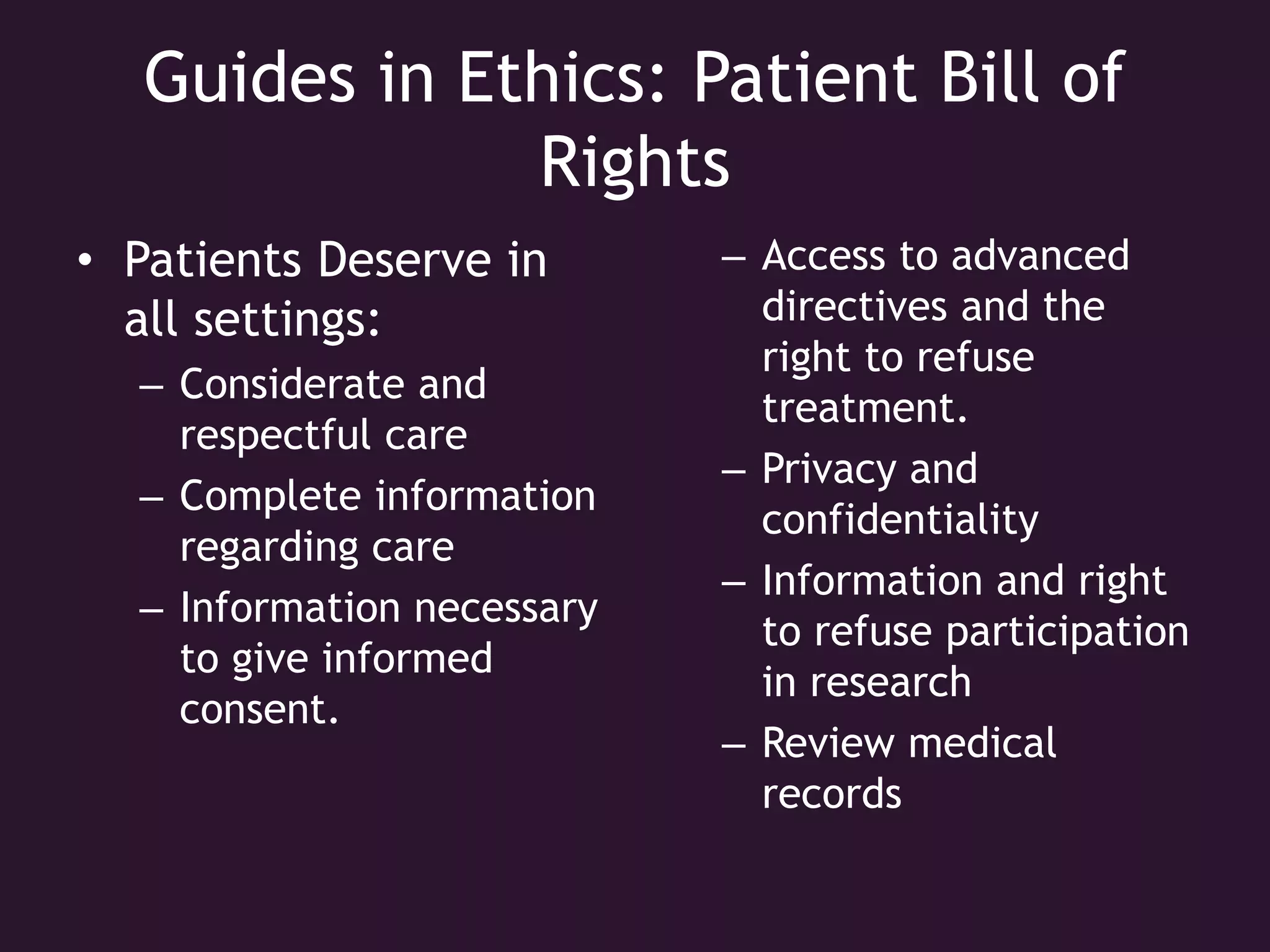
Ethics in healthcare go beyond what is legal and provide moral guidelines to assist in complex decision making. Some examples of ethical issues include deciding who receives organ transplants, discontinuing life support, and how much care to provide uninsured patients. Ethics principles include doing no harm, preserving life, treating all patients equally, respecting patient choices, and maintaining professional standards of care. Patients have rights to considerate care, informed consent, privacy, and participation in advanced directives to refuse treatment.