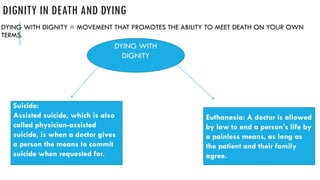
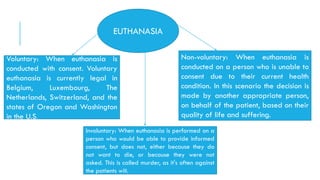
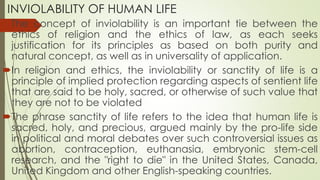
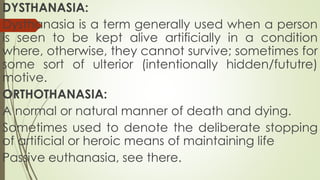
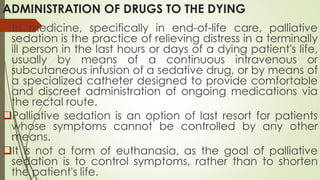
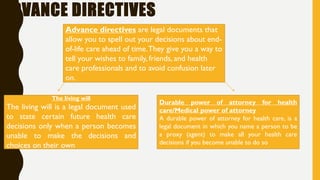
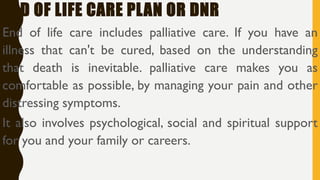
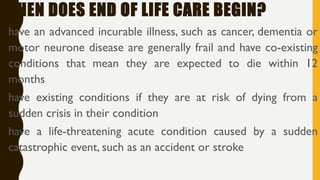
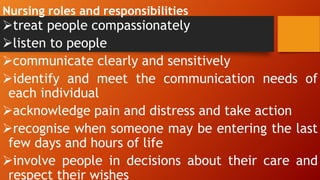
The document discusses bioethical issues related to death and dying, focusing on topics such as euthanasia, palliative care, advance directives, and nursing responsibilities in end-of-life care. It outlines concepts like voluntary and non-voluntary euthanasia, as well as the importance of dignity in dying, while emphasizing the significance of patient choice and ethical decision-making in healthcare. The document further highlights the importance of compassionate care and communication among healthcare professionals when supporting patients and their families during this critical time.