The document discusses diseases of bone, including developmental disorders. It describes four developmental disorders:
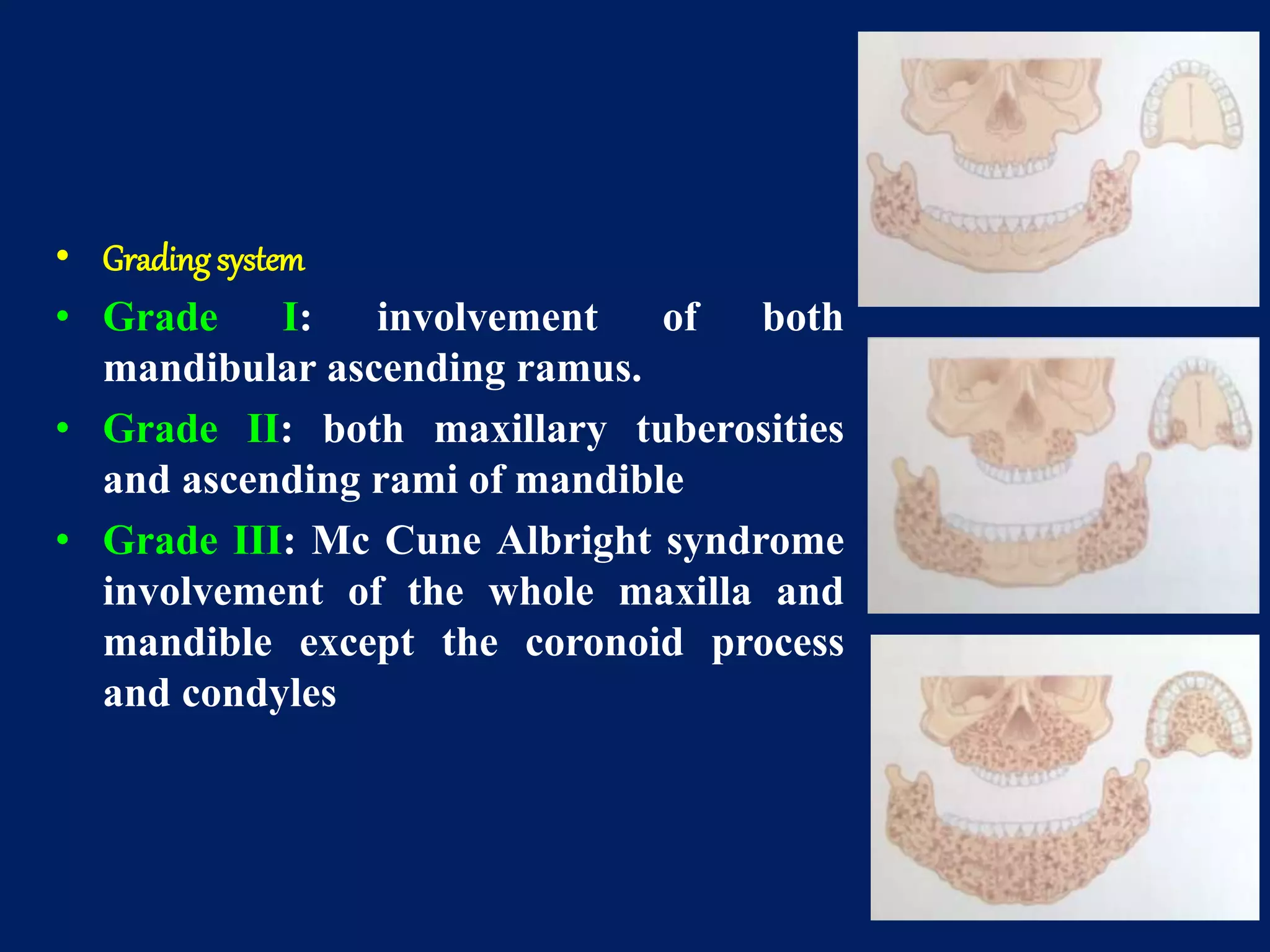
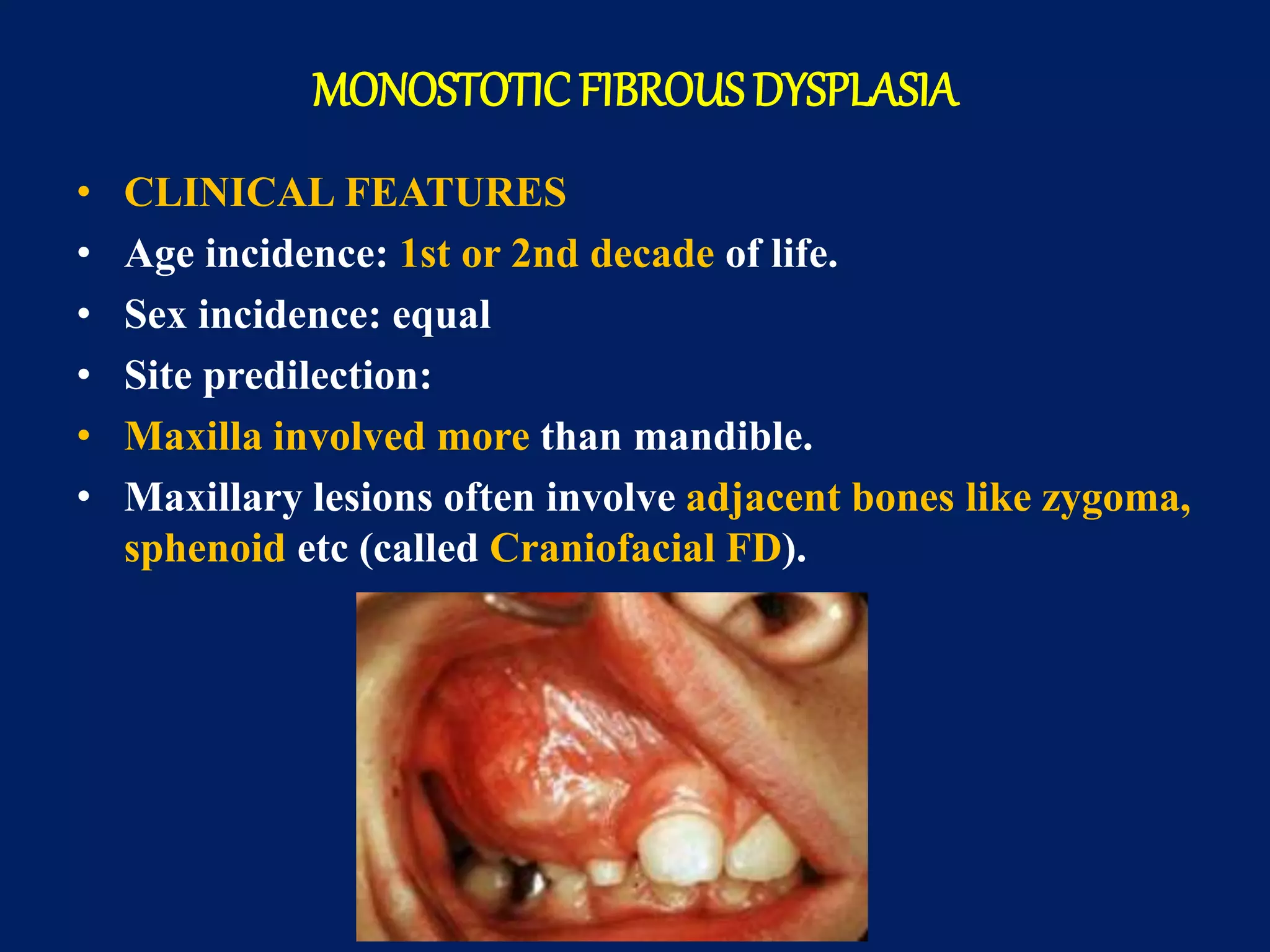
1. Cherubism - A rare jaw condition seen in childhood characterized by bilateral swelling of the jaws due to fibrous dysplasia-like lesions. It is caused by a genetic mutation and lesions typically regress after puberty.
2. Osteopetrosis - A rare disease caused by a defect in bone remodeling resulting in abnormally dense bone that is fragile. It can cause anemia, fractures, and nerve compression.
3. Osteogenesis imperfecta - The most common inherited bone disorder caused by collagen defects, characterized by bone fragility and fractures that easily heal. Other features include blue sclera