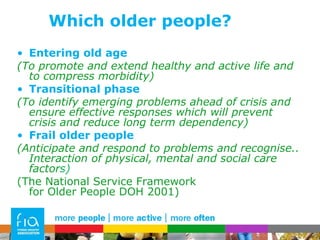
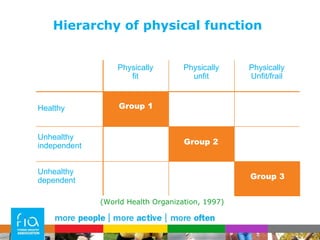
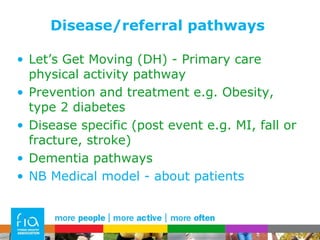
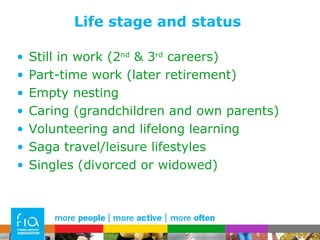
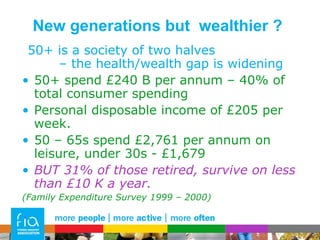
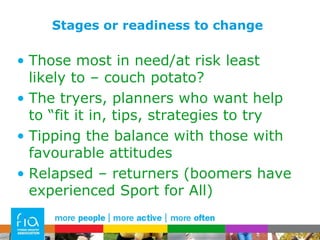
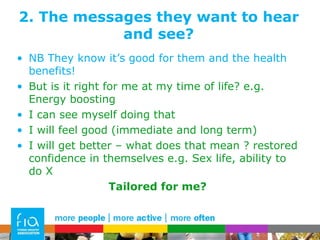
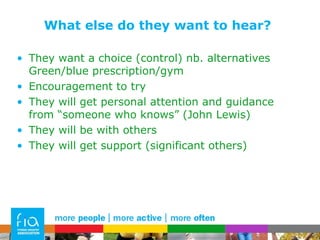
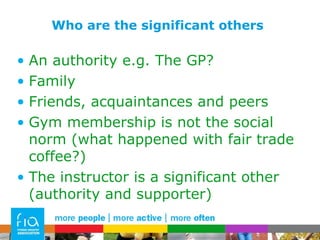
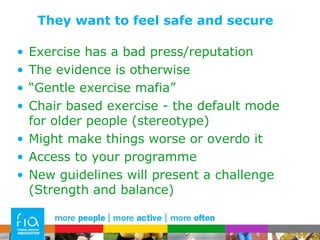
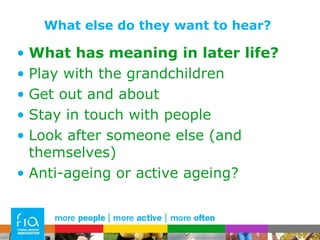
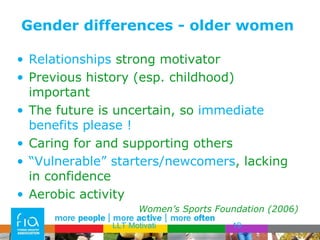
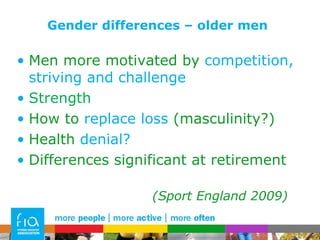
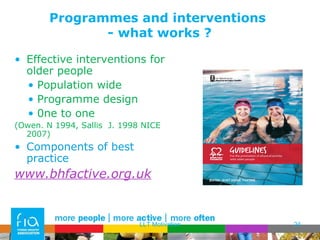
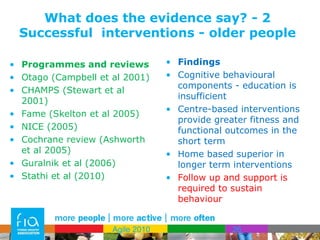
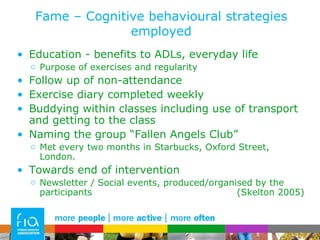
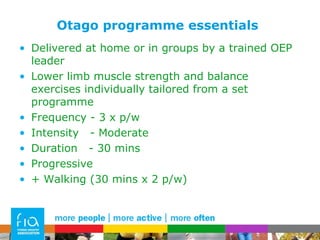
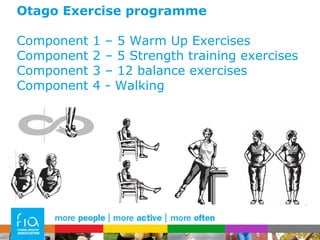
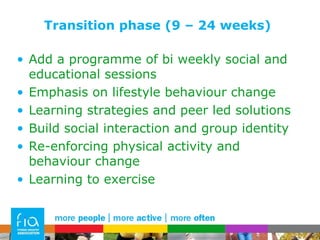
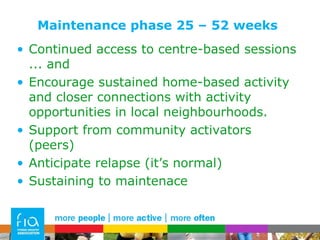
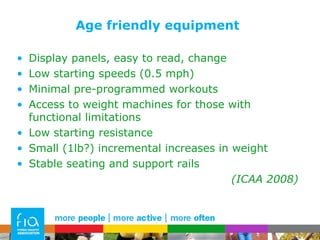
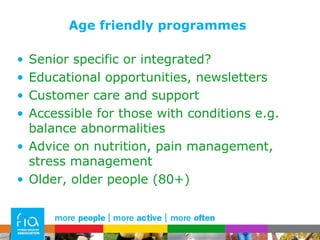
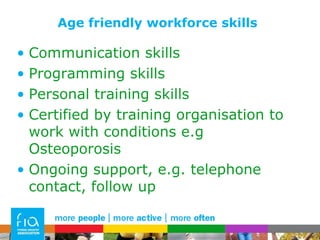
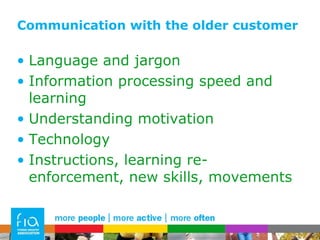
The document discusses engaging older adults in physical activity programs. It covers who to target, important messages to convey, using evidence to design effective programs, and making programs age-friendly. Key points include segmenting the older adult market based on health, life stage, and readiness to change. Messages should focus on benefits, safety, and feeling comfortable. Evidence shows cognitive behavioral strategies and social support increase program adherence and effectiveness. Facilities, equipment, programs, and staff should be tailored to meet the needs and abilities of older adults.








![Thank you for listening [email_address] www.bhfactive.org.uk www.wcaa2012.com www.active-ageing-events.org.uk](https://image.slidesharecdn.com/boblaventurepresentation-110822092455-phpapp01/85/Engaging-the-older-Participant-46-320.jpg)