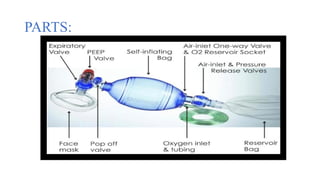
AMBU BAG
A bag valve mask (BVM), sometimes known by the proprietary name AMBU (artificial manual breathing unit) bag or generically as a manual resuscitator or "self-inflating bag", is a hand-held device commonly used to provide positive pressure ventilation to patients who are not breathing or not breathing adequately.
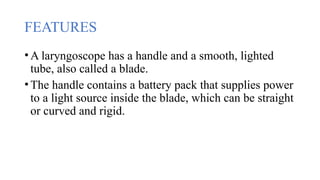
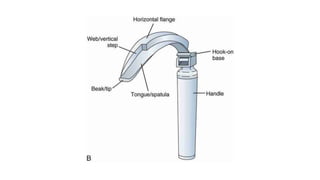
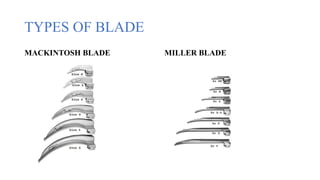
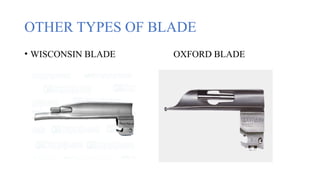
LARYNGOSCOPE
A laryngoscopy is a test healthcare providers perform to examine the larynx (voice box). They perform this test with a laryngoscope, a thin tube with lights, that help them to look closely at the larynx.
Spanish singing teacher manual Garcia invented the laryngoscope in 1855.
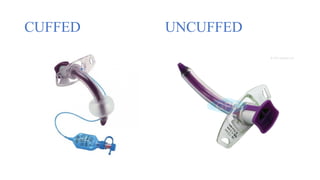
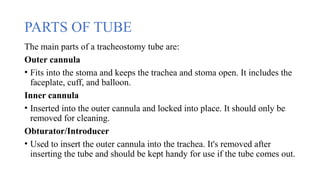
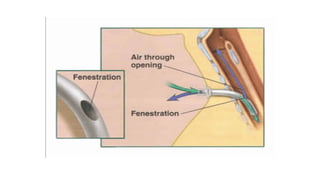
TRACHEOSTOMY TUBE
A tracheostomy tube, also known as a trach tube, is a catheter that's inserted into the trachea (windpipe) to help a person breathe and exchange oxygen and carbon dioxide.
It's used after a tracheostomy, a surgical procedure that creates an opening in the neck into the trachea.
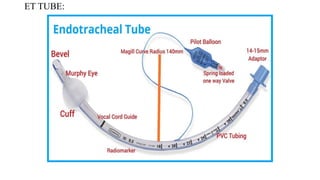
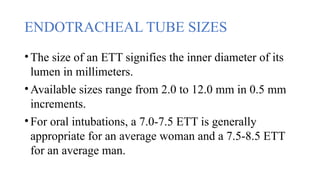
ENDOTRACHEAL TUBE
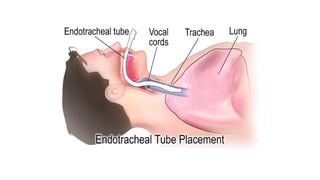
An endotracheal tube (ETT) is a flexible tube that is inserted into the trachea (windpipe) through mouth to help with breathing.
OXYGEN DELIVERY DEVICES
Oxygen can be administered by nasal cannula, mask and tent.
Hyperbaric oxygen therapy involves placing the patient in an airtight chamber with oxygen under pressure.
In the hospital oxygen is supplied to each patient via an outlet in the wall.
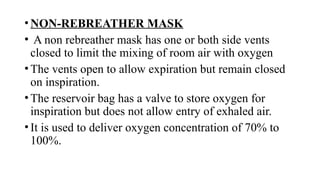
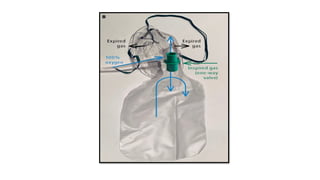
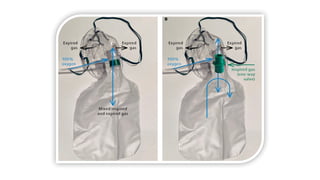
1. LOW-FLOW DEVICES
2. HIGH FLOW DEVICE