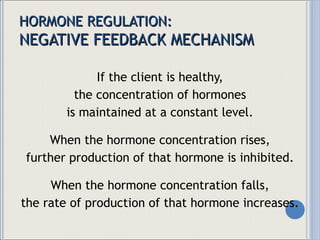
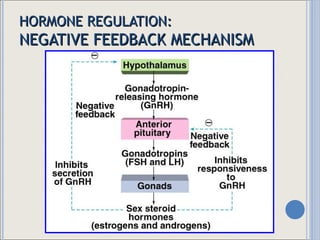
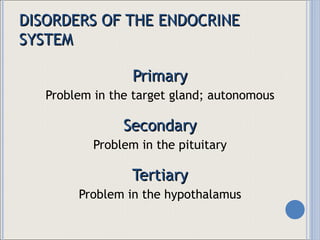
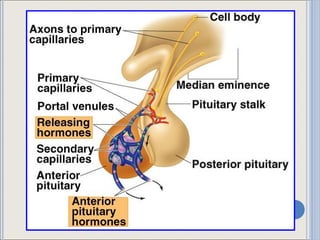
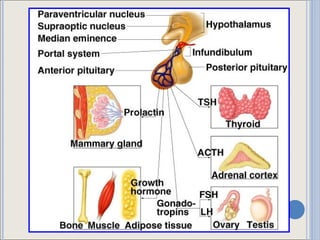
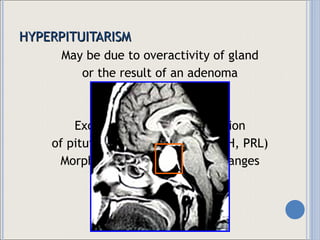
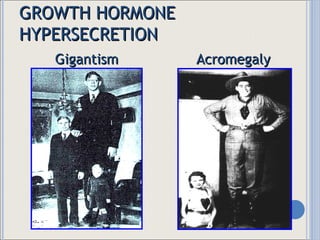
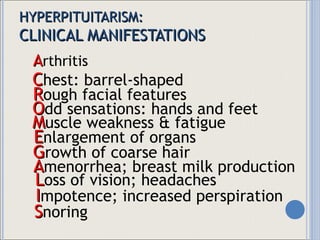
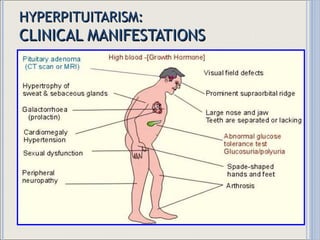
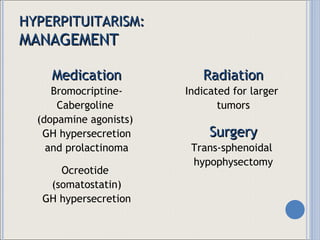
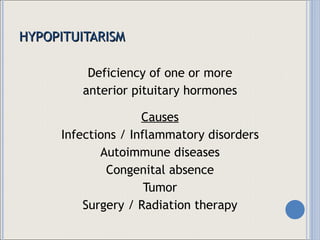
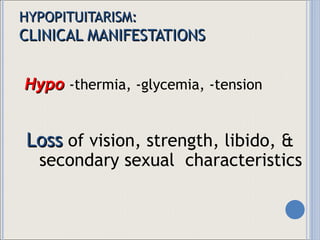
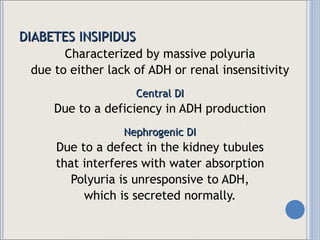
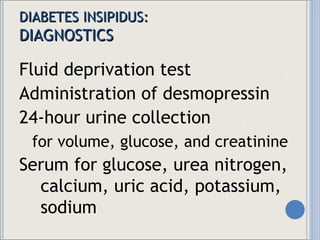
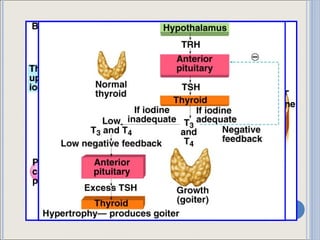
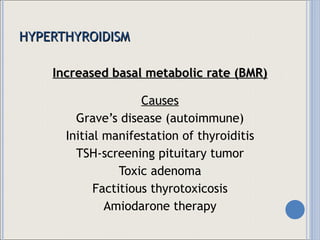
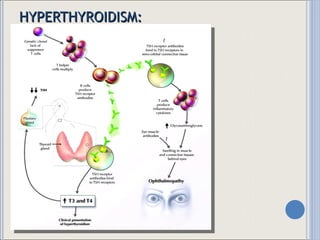
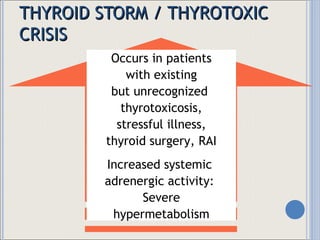
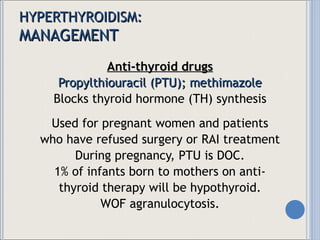
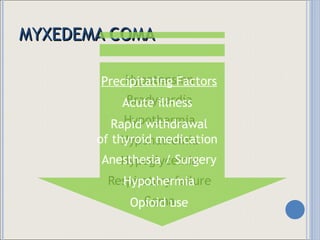
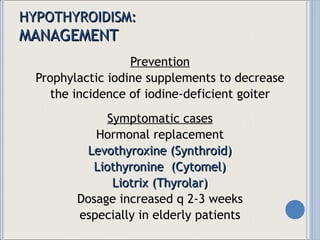
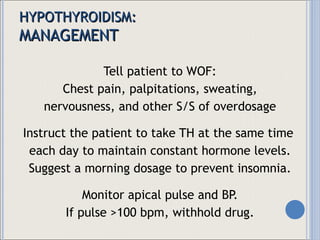
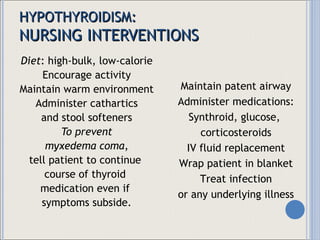
This document summarizes major endocrine disorders, focusing on disorders of the pituitary gland and thyroid gland. It describes the negative feedback mechanism of hormone regulation and classifies endocrine disorders as primary, secondary, or tertiary based on the site of dysfunction. Specific disorders discussed in detail include hyperpituitarism, hypopituitarism, diabetes insipidus, SIADH, hyperthyroidism, hypothyroidism, and myxedema coma. Treatment options for each condition are also outlined.

![TRANS-SPHENOIDAL HYPOPHYSECTOMY Post-surgery nursing care Semi- to high- Fowler’s position Protect from infection and stressful situations Hormone replacement Constant neurologic checks MIOW to check for DI WOF CSF leak Encourage deep-breathing, but not coughing Institute measures to prevent constipation [straining increases ICP]](https://image.slidesharecdn.com/endocrine-disorders-1234399857677955-1/85/Endocrine-Disorders-14-320.jpg)
![HYPOPITUITARISM Simmonds' disease [Panhypopituitarism] Complete absence of pituitary hormones Cachexia: most prominent feature Follows destruction of the pituitary by surgery, infection, injury, or a tumor Sheehan’s syndrome [Post-partum pituitary necrosis] A complication of delivery Results from severe blood loss and hypovolemia Pituitary ischemia](https://image.slidesharecdn.com/endocrine-disorders-1234399857677955-1/85/Endocrine-Disorders-16-320.jpg)
![HYPOPITUITARISM: MANAGEMENT Medication Hormonal substitution [maybe for life] Corticosteroids Levothyroxine Androgen / Estrogen Growth hormone Radiation Indicated for larger tumors Surgery Trans-sphenoidal hypophysectomy](https://image.slidesharecdn.com/endocrine-disorders-1234399857677955-1/85/Endocrine-Disorders-18-320.jpg)
![DIABETES INSIPIDUS: MANAGEMENT Central DI : Desmopressin, Lypressin [intranasal] Vasopressin tannate in oil [IM] Nephrogenic DI : Indomethacin- -hydrochlorothiazide -desmopressin -amiloride Clofibrate, chlorpropamide](https://image.slidesharecdn.com/endocrine-disorders-1234399857677955-1/85/Endocrine-Disorders-24-320.jpg)
![SIADH: DIAGNOSTICS Low serum sodium [<135 mEq/L] Low serum osmolality High urine osmolality [>100 mOsmol/kg] High urine sodium excretion [>20 mmol/L] Normal renal function: low BUN [<10 mg/dL]](https://image.slidesharecdn.com/endocrine-disorders-1234399857677955-1/85/Endocrine-Disorders-26-320.jpg)
![SIADH: MANAGEMENT Maintain fluid balance MIOW Fluid restriction Loop diuretic [If with evidence of fluid overload] Lithium or demeclocycline [Chronic treatment] Maintain Na balance Increased Na intake Emergency treatment of 3% NaCl, followed by furosemide [If serum Na <120, or if patient is seizing] Excessively rapid correction of hyponatremia may cause central pontine myelinolysis!](https://image.slidesharecdn.com/endocrine-disorders-1234399857677955-1/85/Endocrine-Disorders-27-320.jpg)
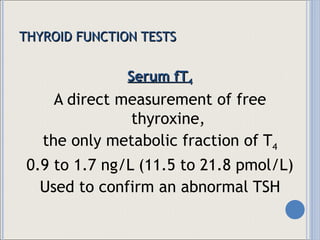
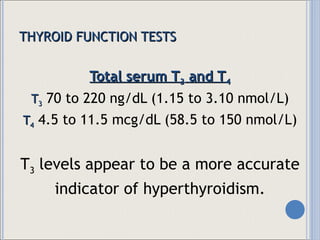
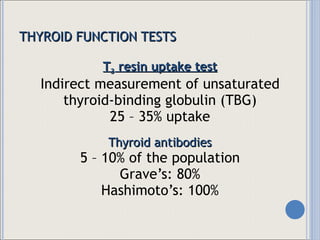
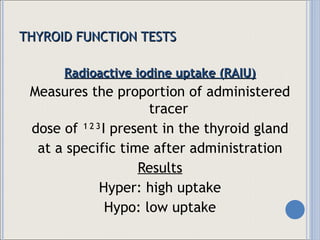
![THYROID FUNCTION TESTS Serum TSH Single best screening test [high sensitivity] 0.38 – 6.15 mcU/mL If TSH is normal, fT 4 should be normal. Screening required beginning 35 years, then q 5 years thereafter Also used for monitoring thyroid hormone replacement therapy](https://image.slidesharecdn.com/endocrine-disorders-1234399857677955-1/85/Endocrine-Disorders-31-320.jpg)
![THYROID FUNCTION TESTS Thyroid scan / Radioscan / Scintiscan Utilizes a gamma camera and radioisotopes 123 I, thallium, americium, technetium-99m [ 99m Tc] pertechnetate Results Hot areas: increased activity Cold areas: decreased activity](https://image.slidesharecdn.com/endocrine-disorders-1234399857677955-1/85/Endocrine-Disorders-35-320.jpg)
![THYROID FUNCTION TESTS Fine-needle aspiration biopsy Sampling of thyroid tissue to detect malignancy Initial test for evaluation of thyroid masses Results Negative [benign] Positive [malignant] Indeterminate [suspicious] Inadequate [non-diagnostic]](https://image.slidesharecdn.com/endocrine-disorders-1234399857677955-1/85/Endocrine-Disorders-37-320.jpg)
![THYROID FUNCTION TESTS Nursing Implications Determine whether the patient has taken medications or agents that contain iodine [antiseptics, multivitamins, cough syrup, amiodarone] because these may alter the test results. Assess for allergy to iodine or shellfish. For scans, tell patient that radiation is only minimal.](https://image.slidesharecdn.com/endocrine-disorders-1234399857677955-1/85/Endocrine-Disorders-38-320.jpg)
![HYPERTHYROIDISM: CLINICAL MANIFESTATIONS G I hypermotility R apid weight loss A pprehension V olume deficit; voracious appetite E xophthalmos; erratic menses S ystolic BP elevated; sweating [tremors, tachycardia, palpitations] in secondary disease in primary disease TSH](https://image.slidesharecdn.com/endocrine-disorders-1234399857677955-1/85/Endocrine-Disorders-40-320.jpg)
![RAI THERAPY : NURSING IMPLICATIONS NPO post-midnight prior to administration [Food may delay absorption] After initial dose: Urine and saliva slightly radioactive x 24H Vomitus highly radioactive x 6-8H Institute full radiation precautions. Instruct the patient to use appropriate disposal methods when coughing and expectorating.](https://image.slidesharecdn.com/endocrine-disorders-1234399857677955-1/85/Endocrine-Disorders-46-320.jpg)
![HYPOTHYROIDISM Causes Chronic autoimmune [Hashimoto’s] thyroiditis Hypothalamic failure to produce TRH Pituitary failure to produce TSH Inborn errors of TH synthesis Thyroidectomy / Radiation therapy Anti-thyroid therapy Iodine deficiency](https://image.slidesharecdn.com/endocrine-disorders-1234399857677955-1/85/Endocrine-Disorders-49-320.jpg)
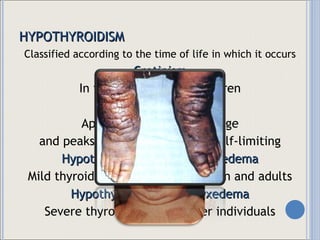
![HYPOTHYROIDISM: CLINICAL MANIFESTATIONS D ry, brittle hair; dry, coarse skin E dema (periorbital) R educed BMR [bradycardia, bradypnea] A pathy; anorexia; anemia I ncreased weight; intolerance to cold L ethargy; loss of libido E nlarged tongue D rooling in secondary disease in primary disease TSH](https://image.slidesharecdn.com/endocrine-disorders-1234399857677955-1/85/Endocrine-Disorders-51-320.jpg)
![HYPERPARATHYROIDISM: MANAGEMENT Surgery to remove adenoma Force fluids; limit dietary calcium intake For life-threatening hypercalcemia: Furosemide Bisphosphonates [Etidroanate (Didrodinel), pamidronate] Calcitonin (Cibacalcin, Miacalcin) Plicamycin (Mithracin) + glucocorticoid Mithramycin](https://image.slidesharecdn.com/endocrine-disorders-1234399857677955-1/85/Endocrine-Disorders-61-320.jpg)
![HYPERTHYROIDISM: MANAGEMENT IV Ca chloride or gluconate [emergency treatment] DOC post-thyroidectomy Oral Ca salts (Ca carbonate or gluconate) Vitamin D supplementation Increase intestinal Ca absorption Dihydrotachysterol, ergocalciferol](https://image.slidesharecdn.com/endocrine-disorders-1234399857677955-1/85/Endocrine-Disorders-64-320.jpg)
![HYPOPARATHYROIDISM Parathormone injections [in acute attacks] WOF allergies Diet: High-calcium [spinach], low-phosphate [milk, cheese, egg yolks] Al(OH) 2 , Gelusil, Amphogel p.c. Pentobarbital (Nembutal) [calm environment]](https://image.slidesharecdn.com/endocrine-disorders-1234399857677955-1/85/Endocrine-Disorders-66-320.jpg)

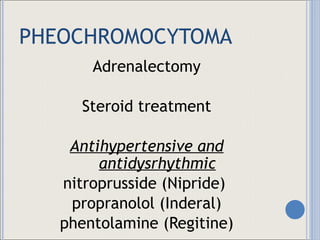
![PHEOCHROMOCYTOMA MBP / MIO Fluid replacements Decrease environmental stimulation Maintenance doses of steroids Follow-up check up 24-hour urine specimens [VMA and catecholamine studies] Avoid : coffee, chocolate, beer, wine, citrus fruit, bananas, and vanilla 24h before test](https://image.slidesharecdn.com/endocrine-disorders-1234399857677955-1/85/Endocrine-Disorders-75-320.jpg)
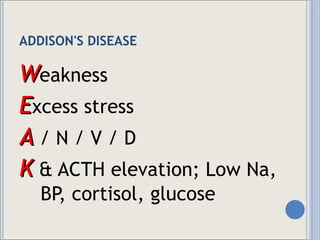
![ADDISON'S DISEASE VS, weight, and serum glucose level 24-hour urine specimens [LOW 17- hydroxycorticosteroids & 17-ketosteroids] Electrolyte levels: K; Na Bronze-skin Changes in energy or activity](https://image.slidesharecdn.com/endocrine-disorders-1234399857677955-1/85/Endocrine-Disorders-86-320.jpg)
![ADDISON'S DISEASE MVS [4x / day] Infection, Addisonian crisis, dehydration MIOW / MBP / MBG Give steroids with milk or an antacid Avoid : Contacts & Stress](https://image.slidesharecdn.com/endocrine-disorders-1234399857677955-1/85/Endocrine-Disorders-88-320.jpg)

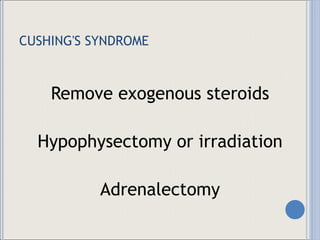
![CUSHING'S SYNDROME MVS, MIOW, MBP, MBG Electrolyte levels: Na & K Urine specimens [LOW 17- hydroxycorticosteroids & 17-ketosteroids] Physical appearance Changes in coping & sexuality [verbalization] Stress reduction](https://image.slidesharecdn.com/endocrine-disorders-1234399857677955-1/85/Endocrine-Disorders-96-320.jpg)
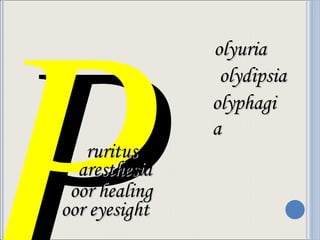
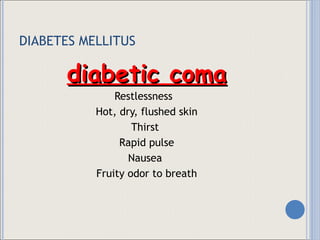
![DIABETES MELLITUS Insulin resistance [GDM, age] Failure in production Blockage of insulin supply Autoimmune response Excess body fat Heredity](https://image.slidesharecdn.com/endocrine-disorders-1234399857677955-1/85/Endocrine-Disorders-98-320.jpg)
![DIABETES MELLITUS Type I [juvenile ]/IDDM Type II [adult- onset type]/ NIDDM gradual onset diet and exercise obesity Pancreatectomy, Cushing's syndrome, drugs](https://image.slidesharecdn.com/endocrine-disorders-1234399857677955-1/85/Endocrine-Disorders-99-320.jpg)
![DIABETES MELLITUS Diet complex CHO [50% to 60%] water-soluble fiber oat, bran, peas, beans, pectin-rich FV CHON [12% to 20%] 60 and 85 g CHOO [<30%] 70 to 90 g/day / MUFA](https://image.slidesharecdn.com/endocrine-disorders-1234399857677955-1/85/Endocrine-Disorders-104-320.jpg)
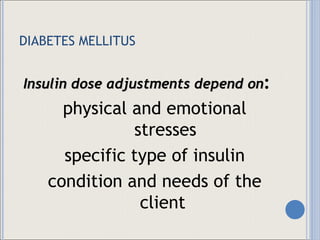
![Insulin Onset Peak Duration Ultra rapid acting insulin analog (humalog) 10-15 min 1 H 3 H SAI (humulin regular) ½ - 1 H 2-4 H 4-6 (8) H IAI (humulin lente, Humulin NPH) 3-4 H 4-12 H 16-20 H LAI (Protamine zinc, humulin ultralente) 6-8 H 12-16 H 20-30 H Premixed insulin (NPH-regular [80-20, 70-30, 50-50]) ½-1 H 2-12 H 18-24 hrs Insulin glargine (Lantus ) Slower than NPH No Peak 24 H](https://image.slidesharecdn.com/endocrine-disorders-1234399857677955-1/85/Endocrine-Disorders-106-320.jpg)
![DIABETES MELLITUS Somogyi effect Epinephrine & Glucagon Glycogenolysis [iatrogenically-induced hyperglycemia] Lowering insulin dosage at night MBG](https://image.slidesharecdn.com/endocrine-disorders-1234399857677955-1/85/Endocrine-Disorders-107-320.jpg)
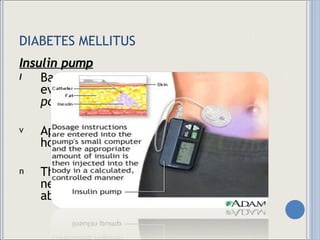

![DIABETES MELLITUS Other therapies include: pancreas islet cell grafts pancreas transplants implantable insulin pumps cyclosporin [Sandimmune, Neoral]](https://image.slidesharecdn.com/endocrine-disorders-1234399857677955-1/85/Endocrine-Disorders-115-320.jpg)
![DIABETES MELLITUS MBG [done pc and hs ] + HbA1C MBP + weight Renal function + MIO Eye examination](https://image.slidesharecdn.com/endocrine-disorders-1234399857677955-1/85/Endocrine-Disorders-116-320.jpg)
![DIABETES MELLITUS diet & weight ketonuria note infection legs / feet / toenails check [keep in between toes dry] acceptance & understanding](https://image.slidesharecdn.com/endocrine-disorders-1234399857677955-1/85/Endocrine-Disorders-118-320.jpg)


![K etoacidosis U rinary changes S unken eyeballs S kin is warm & flushed M embranes are dry A rrhythmias U pset GI system L ow BP S aline solution Rx : Regular insulin drip 0.9% or 0.45% NSS 1:1 [100U:100cc] Nursing care: Check glucose 250-300 mg/dL [q30-60mins] 250 mg/dL DC the drip](https://image.slidesharecdn.com/endocrine-disorders-1234399857677955-1/85/Endocrine-Disorders-126-320.jpg)
![NON K etosis is absent E lectrolyte imbalance [K + decrease] T hirst O btundation T reat with regular insulin drip I nitiate diet C orrect hyperglycemia](https://image.slidesharecdn.com/endocrine-disorders-1234399857677955-1/85/Endocrine-Disorders-127-320.jpg)
![N ormal creatinine? E rythrocyte sedimentation rate [ESR: 0-20 mm/hr] P oor glycemic control H emodialysis R estrict: Na + , CHON, K + , weight O utput & input (MIO) N o symptoms](https://image.slidesharecdn.com/endocrine-disorders-1234399857677955-1/85/Endocrine-Disorders-128-320.jpg)
![R educed O 2 in the eye E levated sugar & BP T ension is high in the retina I ncreased lens opacity N O eyesight A nnual eye exam [every 6-12 months]](https://image.slidesharecdn.com/endocrine-disorders-1234399857677955-1/85/Endocrine-Disorders-129-320.jpg)