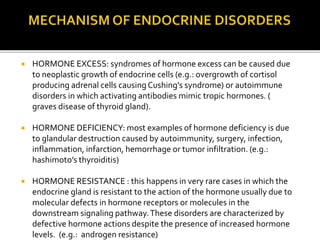
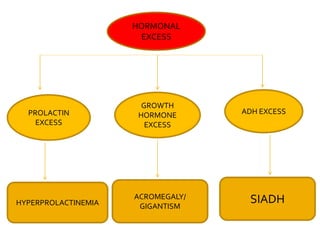
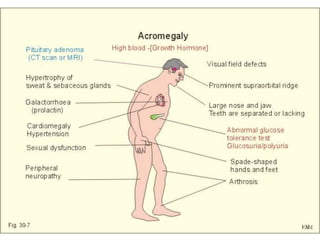
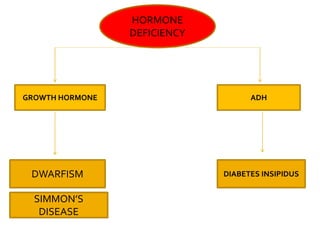
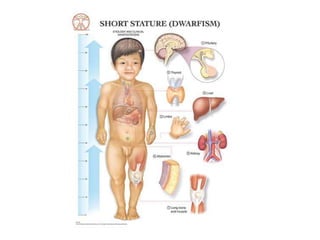
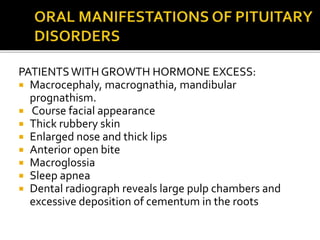
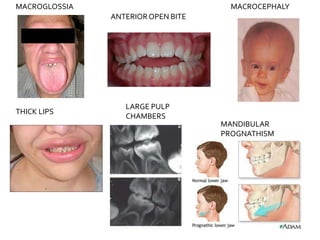
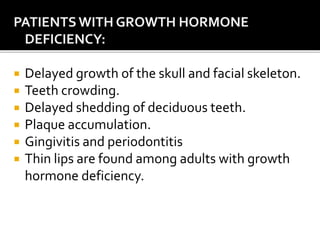
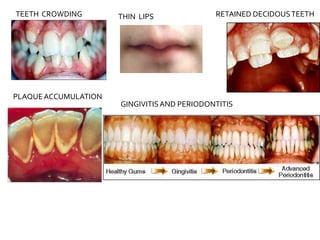
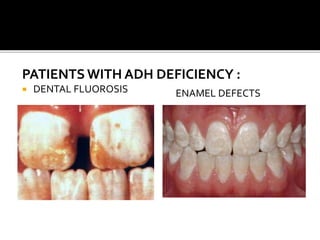
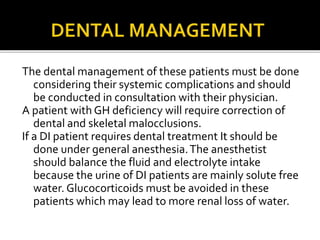
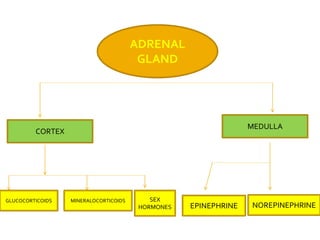
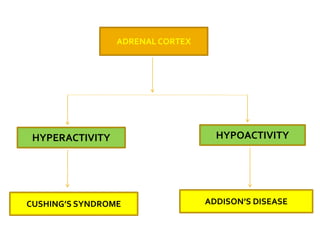
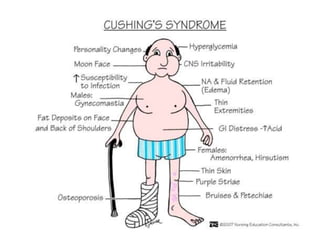
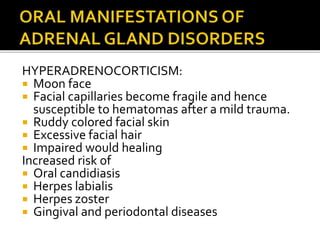
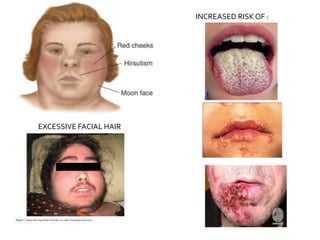
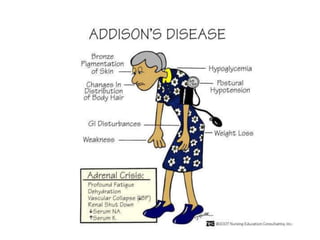
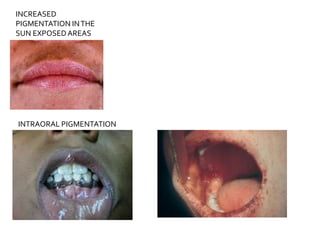
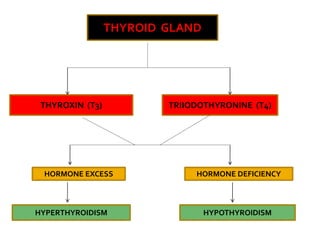
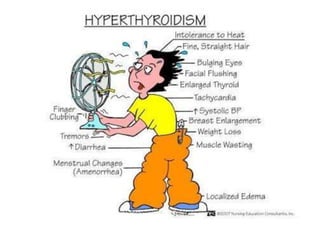
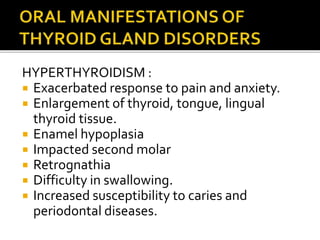
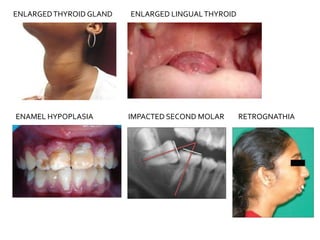
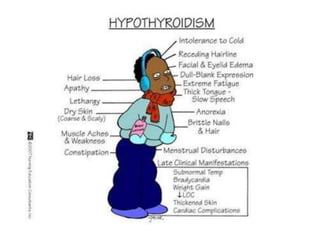
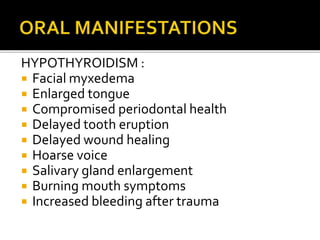
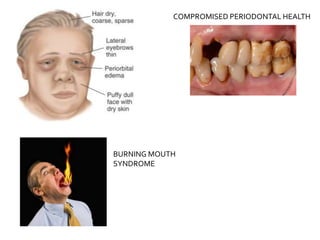
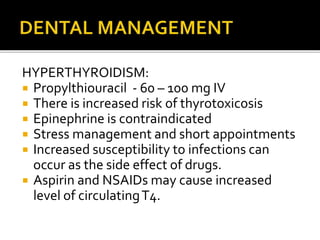
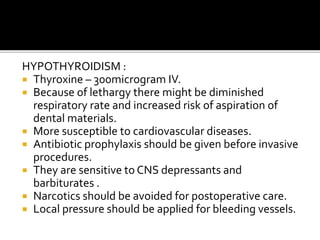
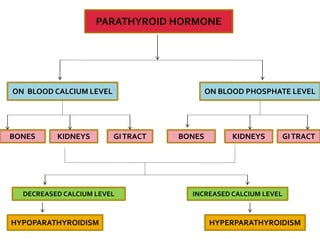
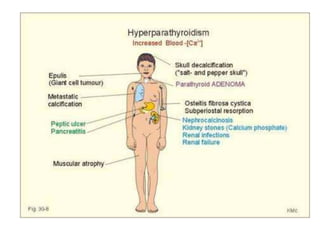
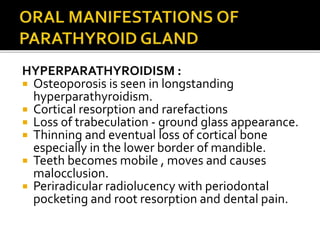
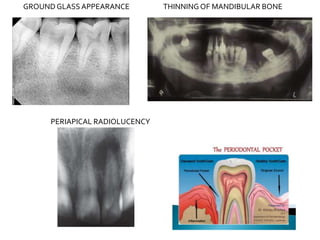
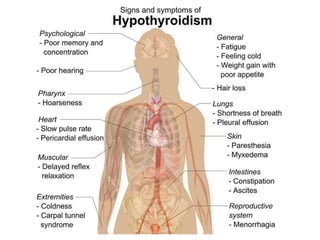
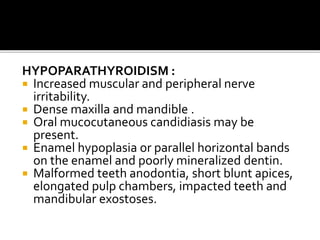
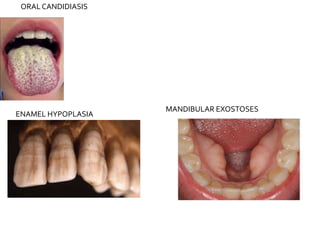
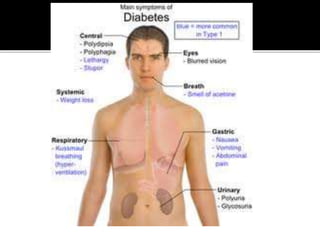
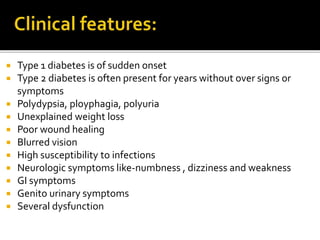
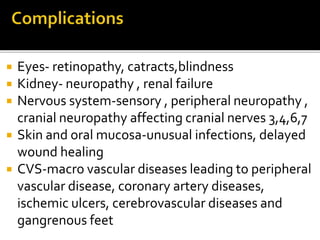
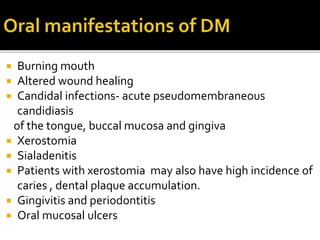
This document discusses dental considerations for patients with endocrine diseases. It covers hormone excess, deficiency, and resistance related to the pituitary gland, adrenal gland, thyroid gland, and parathyroid glands. Key points include increased risk of infections for patients on high-dose steroids (Cushing's); need for IV glucocorticoids before dental work in Addison's disease; risks of aspiration and bleeding in hypothyroidism; increased caries and mobility in hyperparathyroidism; and increased infections and delayed healing in diabetes. Systemic treatment needs and dental management strategies are provided for each condition.