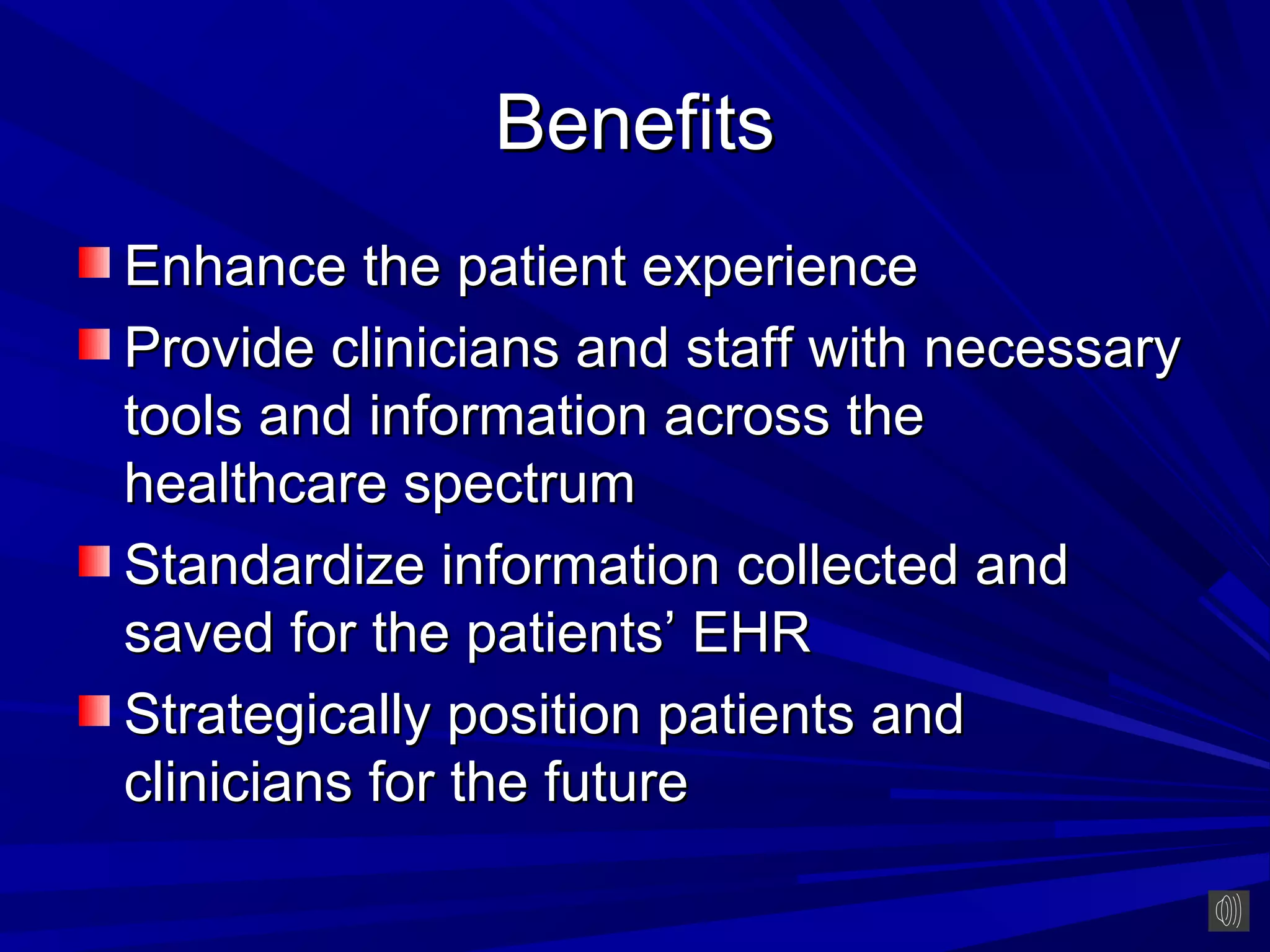
This document discusses building consensus for electronic health records (EHRs). It begins by defining EHRs and distinguishing them from electronic medical records (EMRs). The document outlines the benefits of EHRs, such as reducing medical errors, improving patient outcomes, and empowering patients. It also discusses meaningful use standards and key aspects of EHR implementation like computerized physician order entry. Overall, the document emphasizes that successful EHR adoption requires thorough preparation, customized training, and comprehensive security planning.