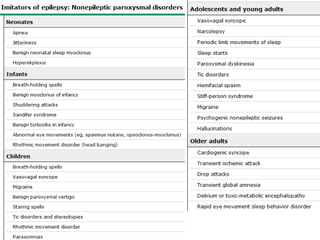
This document discusses the use and interpretation of electroencephalography (EEG) in evaluating patients for possible epilepsy. It makes several key points:
1. EEG alone cannot be used to definitively diagnose or rule out epilepsy, as abnormal EEG patterns can be caused by various neurological conditions, and not all epilepsy cases show EEG abnormalities.
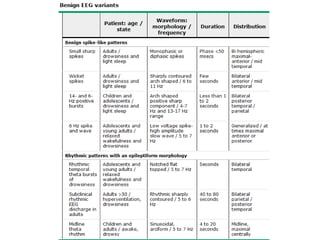
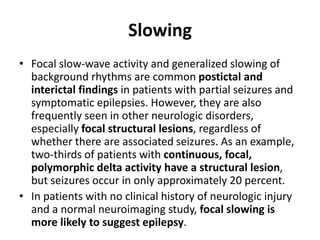
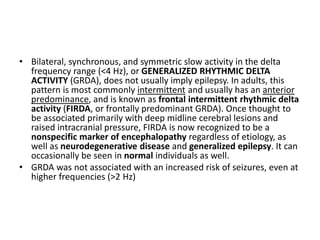
2. Certain EEG findings like interictal epileptiform discharges (IEDs) are strongly associated with epilepsy, while nonspecific findings like slowing are less so.
3. The sensitivity of EEG for detecting epilepsy depends on factors like the number of studies, study duration, seizure frequency, and use of activation procedures.
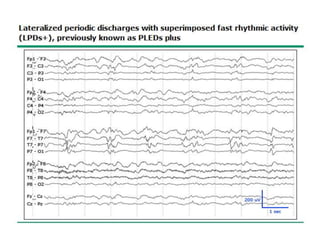
4. Specific EEG patterns like lateralized periodic
![EEG FINDINGS IN PATIENTS WITH
EPILEPSY
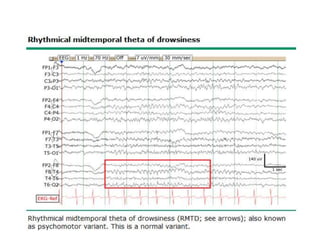
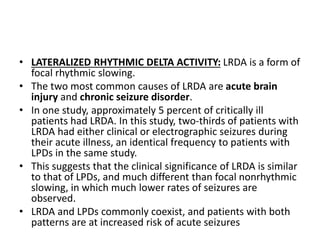
• Different EEG findings are variably associated with
epilepsy.
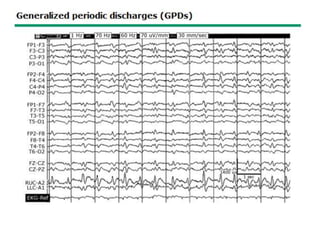
– Examples of epileptiform activity include interictal
epileptiform discharges (IEDs), lateralized periodic
discharges (LPDs; previously known as periodic lateralized
epileptiform discharges [PLEDs], and generalized periodic
discharges (GPDs).](https://image.slidesharecdn.com/eeg-201009135945/85/Eeg-basics-part-1-8-320.jpg)
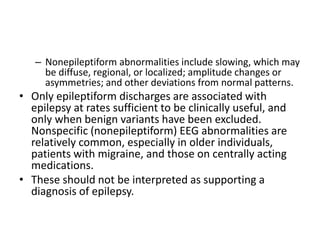
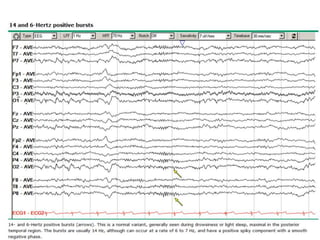
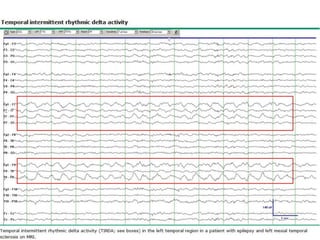
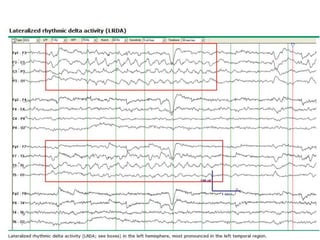
![• Occipital intermittent rhythmic delta activity (OIRDA) is more
common in young children and is rarely seen in patients older than
15 years. It is a frequent interictal finding in generalized epilepsy
syndromes, occurring in 15 to 38 percent of all patients with
childhood absence epilepsy, and implies a good prognosis.
• Temporal intermittent rhythmic delta activity (TIRDA) is a
particular form of focal slowing (and a subtype of lateralized
rhythmic delta activity [LRDA]; that is specific for temporal lobe
localization in patients with refractory epilepsy. TIRDA is observed in
as many as 25 to 40 percent of patients being evaluated for
temporal lobe resection. TIRDA is often associated with temporal
IEDs and has a high positive predictive value for temporal lobe
localization in patients with refractory epilepsy.](https://image.slidesharecdn.com/eeg-201009135945/85/Eeg-basics-part-1-26-320.jpg)

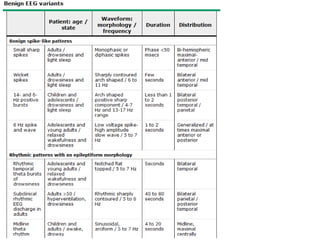
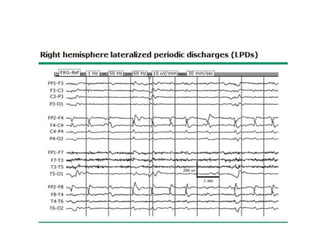
![Sleep and sleep deprivation
• Sleep is a neurophysiologic activator of epilepsy; 20 to 40 percent
of epilepsy patients with an initial normal recording will have IEDs
on a subsequent recording that includes sleep.
• Sleep is sometimes captured on a routine EEG, but sleep
deprivation increases this likelihood.
• Sleep is also usually captured on prolonged EEG monitoring and,
alternatively, can be induced by administration of a sedative,
usually chloral hydrate.
• Sleep deprivation appears to increase IEDs to an extent not fully
explained by the greater chance of recording sleep. One study
found that the additional yield of a sleep-deprived EEG was similar
whether or not sleep was recorded [83].
• The sleep-deprived patients were also more likely to have a seizure
during the EEG compared with the sedated patients.](https://image.slidesharecdn.com/eeg-201009135945/85/Eeg-basics-part-1-34-320.jpg)