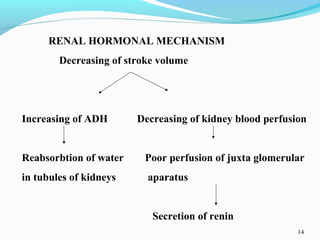
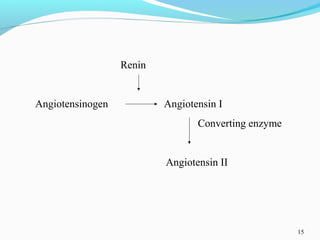
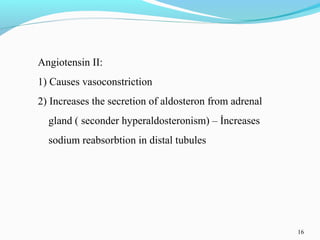
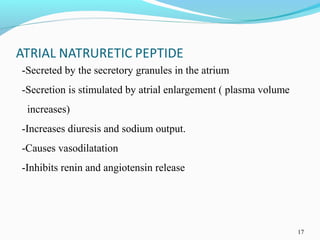
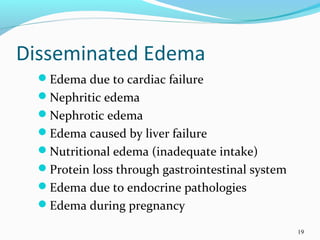
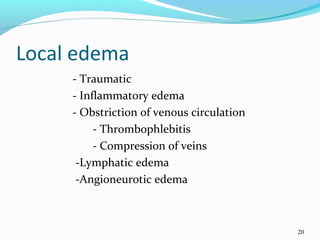
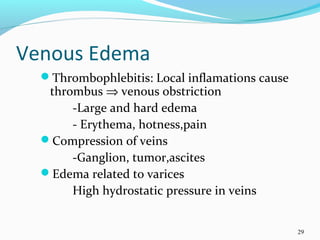
The document discusses edema, which is an increase in fluid volume in body tissues. It notes that 75% of body weight is water, with 50% being intracellular volume, 20% interstitial volume, and 5% intravascular volume. Edema can be local, such as pulmonary or cerebral edema, or disseminated, involving an increase in interstitial fluid volume. The pathogenesis of edema involves capillary permeability, hydrostatic pressure, oncotic pressure, tissue resistance, lymphatic drainage, and renal/hormonal factors.