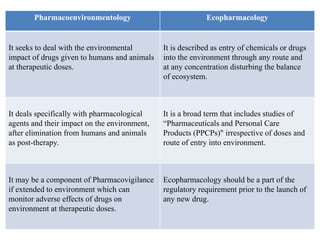
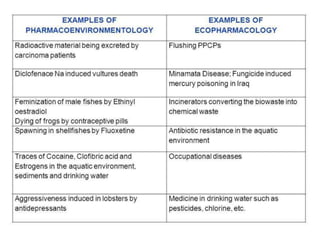
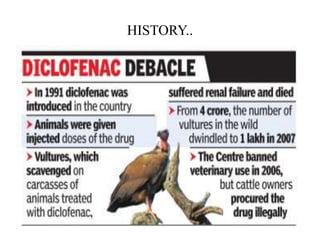
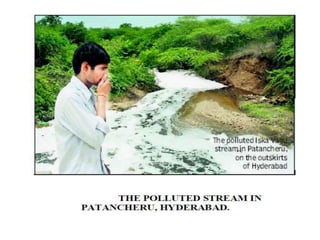
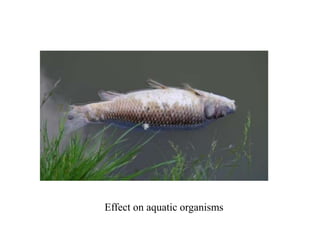
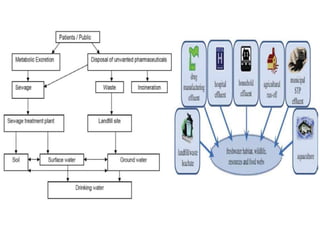
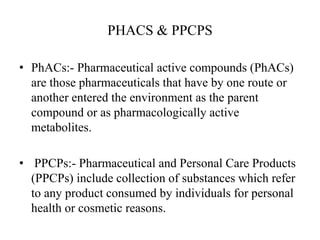
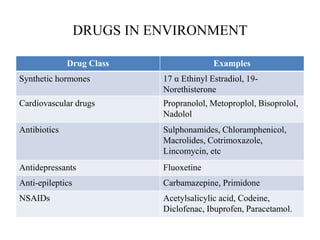
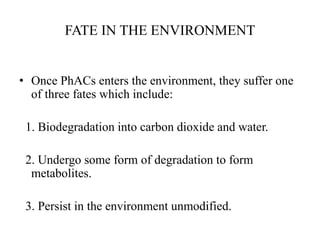
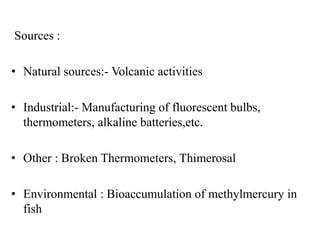
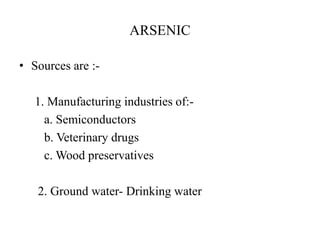
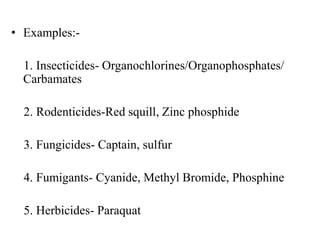
This document provides an overview of ecopharmacology, which is the study of the effects of pharmaceuticals and personal care products on the environment. It discusses how drugs enter the environment through various routes like excretion, disposal down drains, and agricultural runoff. Once in the environment, drugs can biodegrade, form metabolites, or persist unmodified. Persistent pharmaceutical pollutants can accumulate and have effects on aquatic organisms and microbial communities. The document also outlines some of the ways drugs can impact ecosystems and human health, such as endocrine disruption, autoimmune diseases, epigenetic effects, and toxicity of heavy metals like lead, mercury, and arsenic.