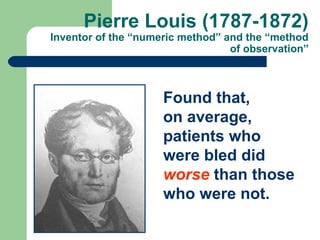
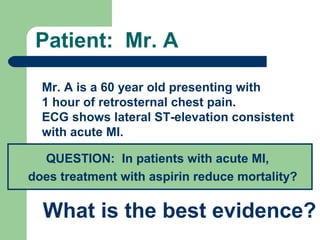
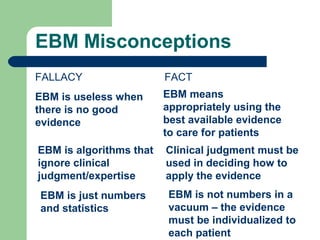
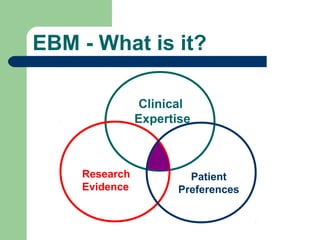
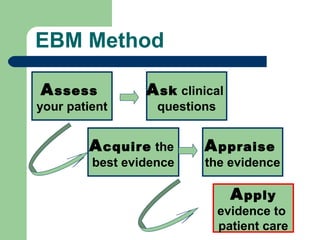
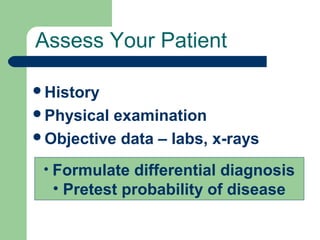
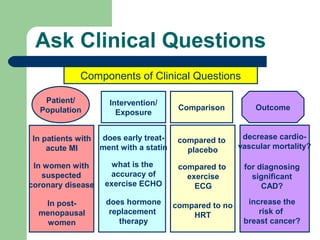
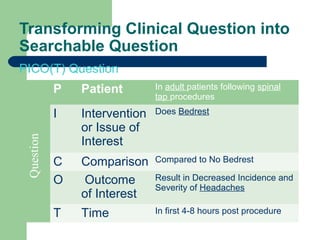
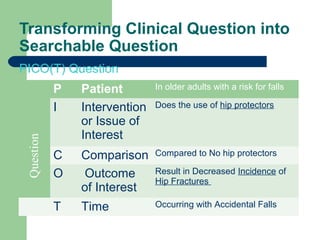
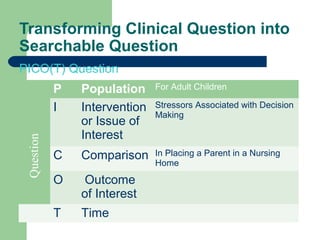
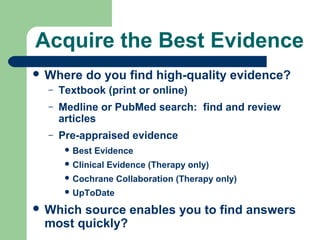
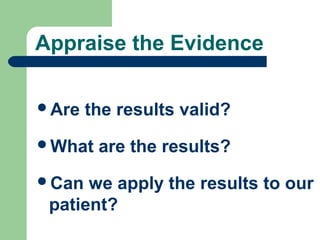
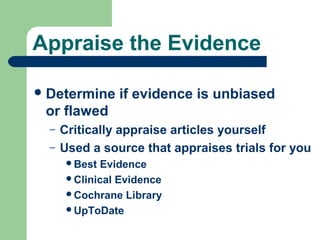
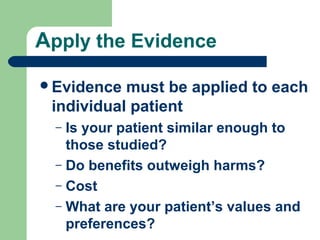
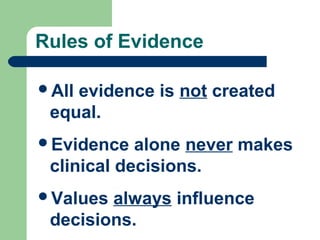
The document provides an introduction to evidence-based medicine (EBM). It defines EBM as an approach to clinical decision-making that integrates the best available research evidence, patient values and clinical expertise. The document outlines the key steps of EBM, including asking clinical questions, acquiring evidence from reliable sources, appraising the quality of the evidence, and applying it to individual patients. EBM aims to improve healthcare quality by minimizing ineffective, unsafe practices and promoting interventions that are supported by scientific evidence.