This document provides an overview of evidence-based practice and the steps involved. It discusses:
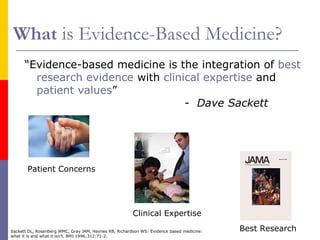
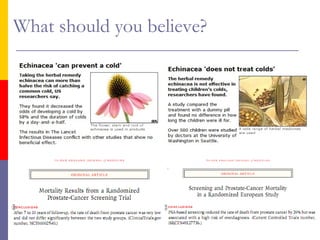
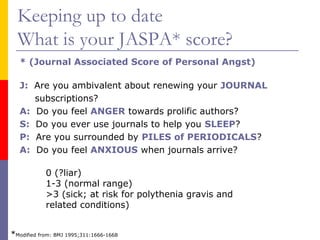
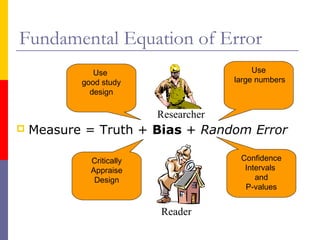
1) What evidence-based medicine is and its key principles of integrating the best research evidence with clinical expertise and patient values.
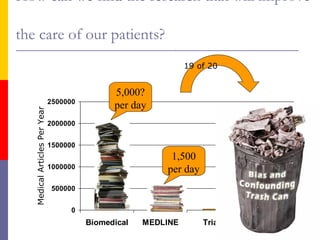
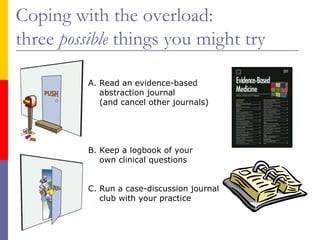
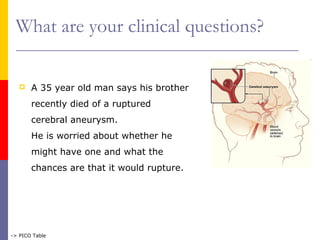
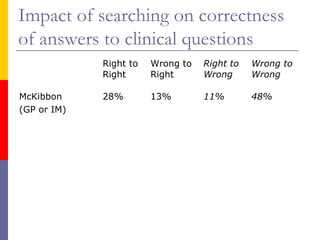
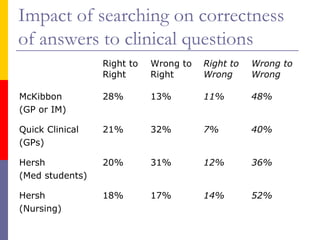
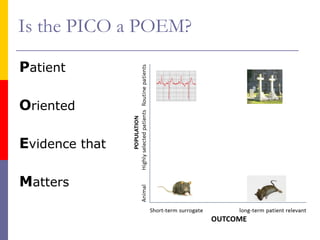
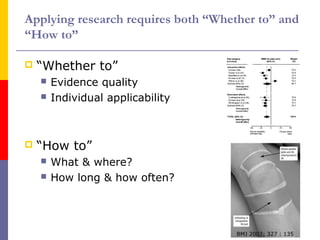
2) The four steps of evidence-based practice: formulating a clinical question, searching for evidence, appraising the research, and applying to individual patients.
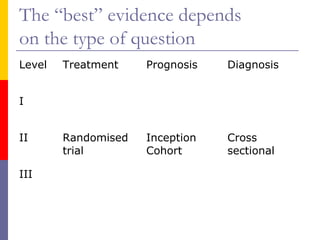
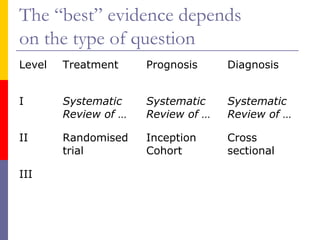
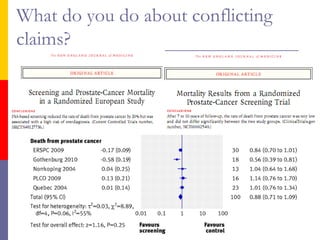
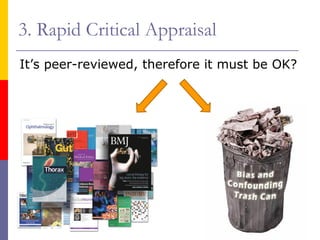
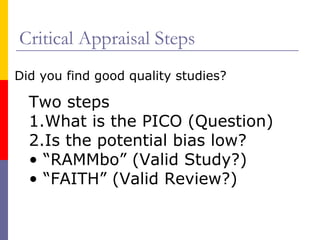
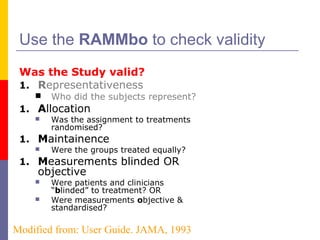
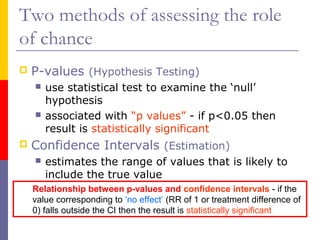
3) Tools for critically appraising different types of research studies, such as randomized trials and systematic reviews, to assess their validity and potential for bias.