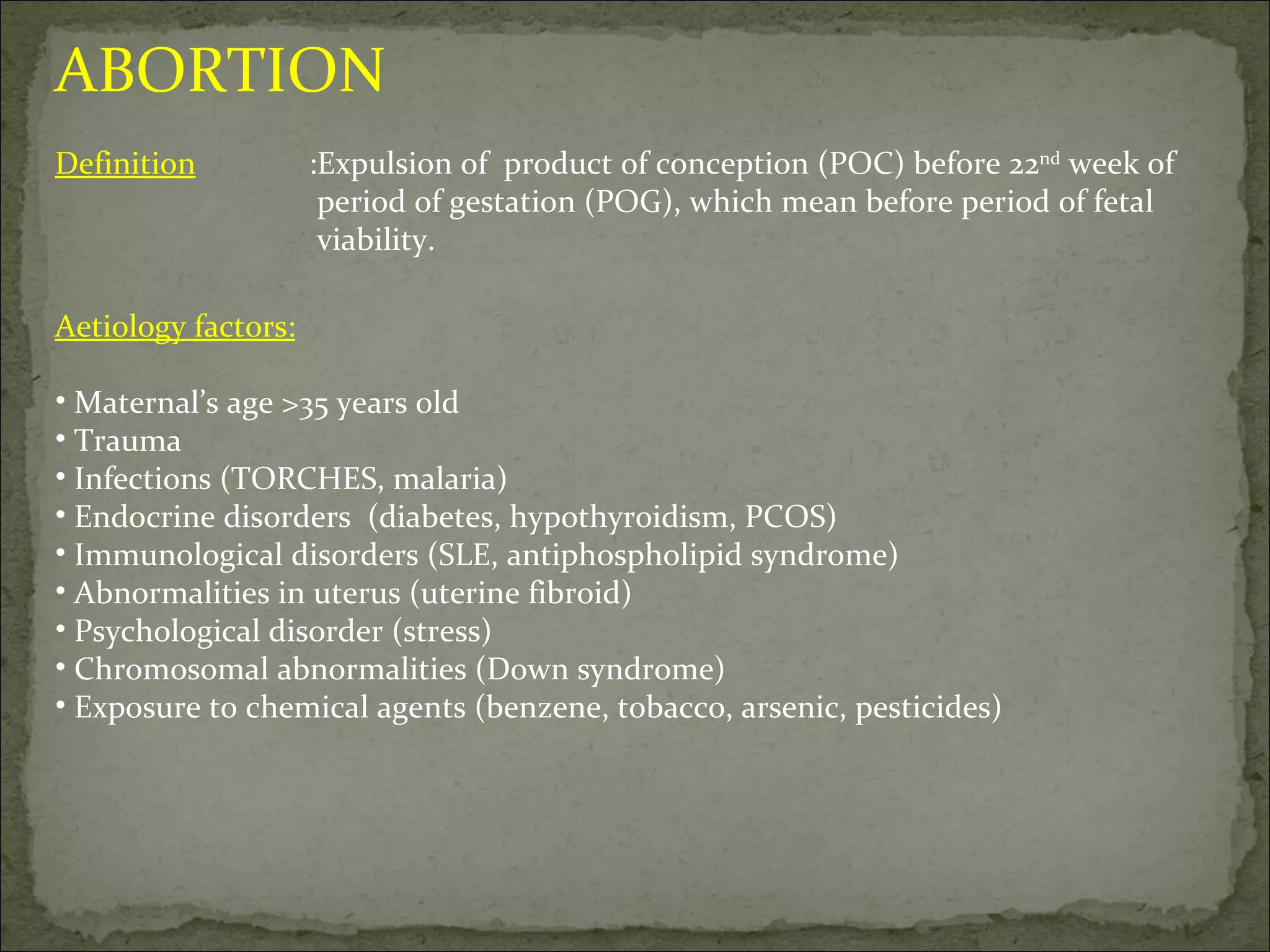
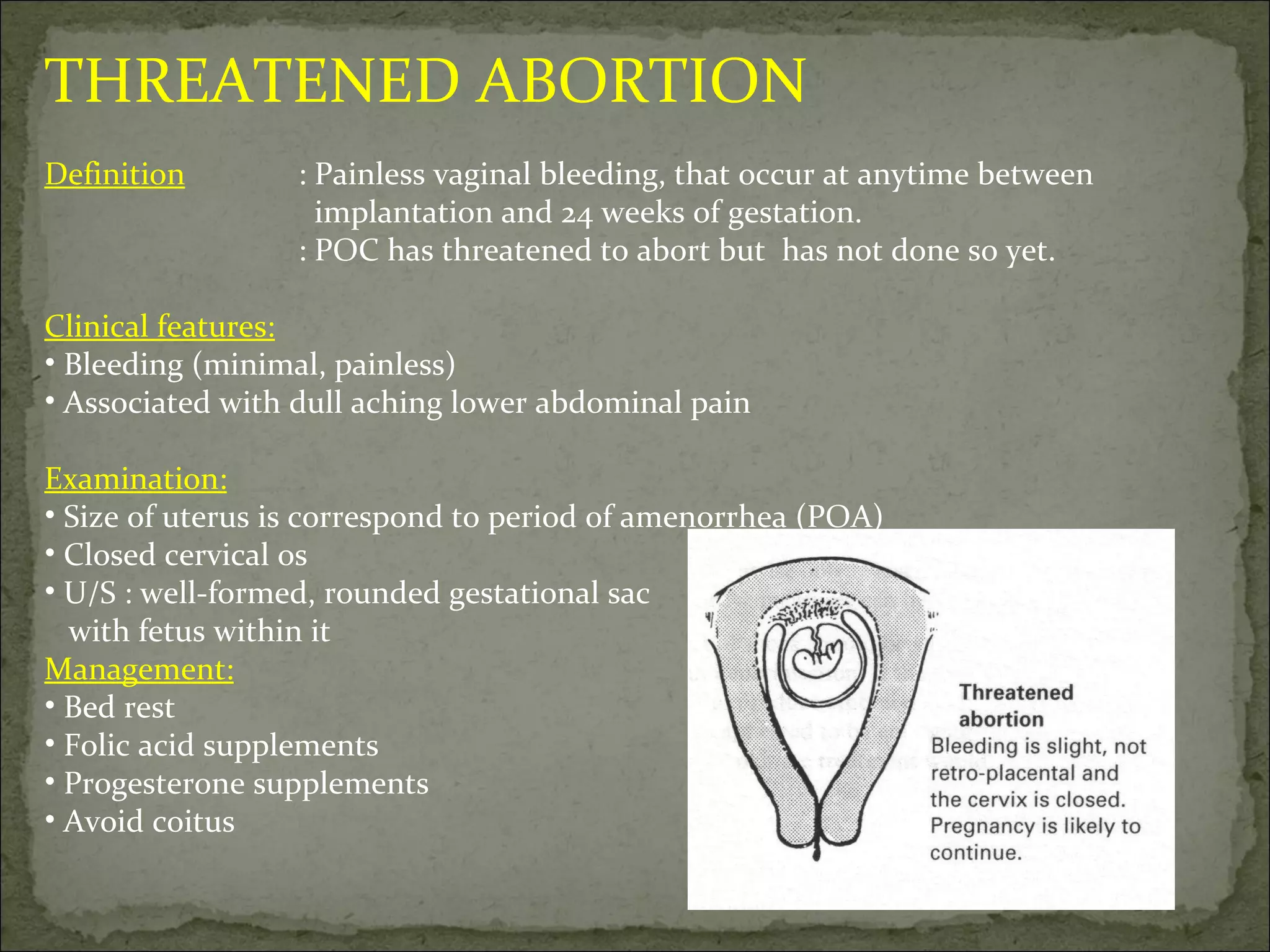
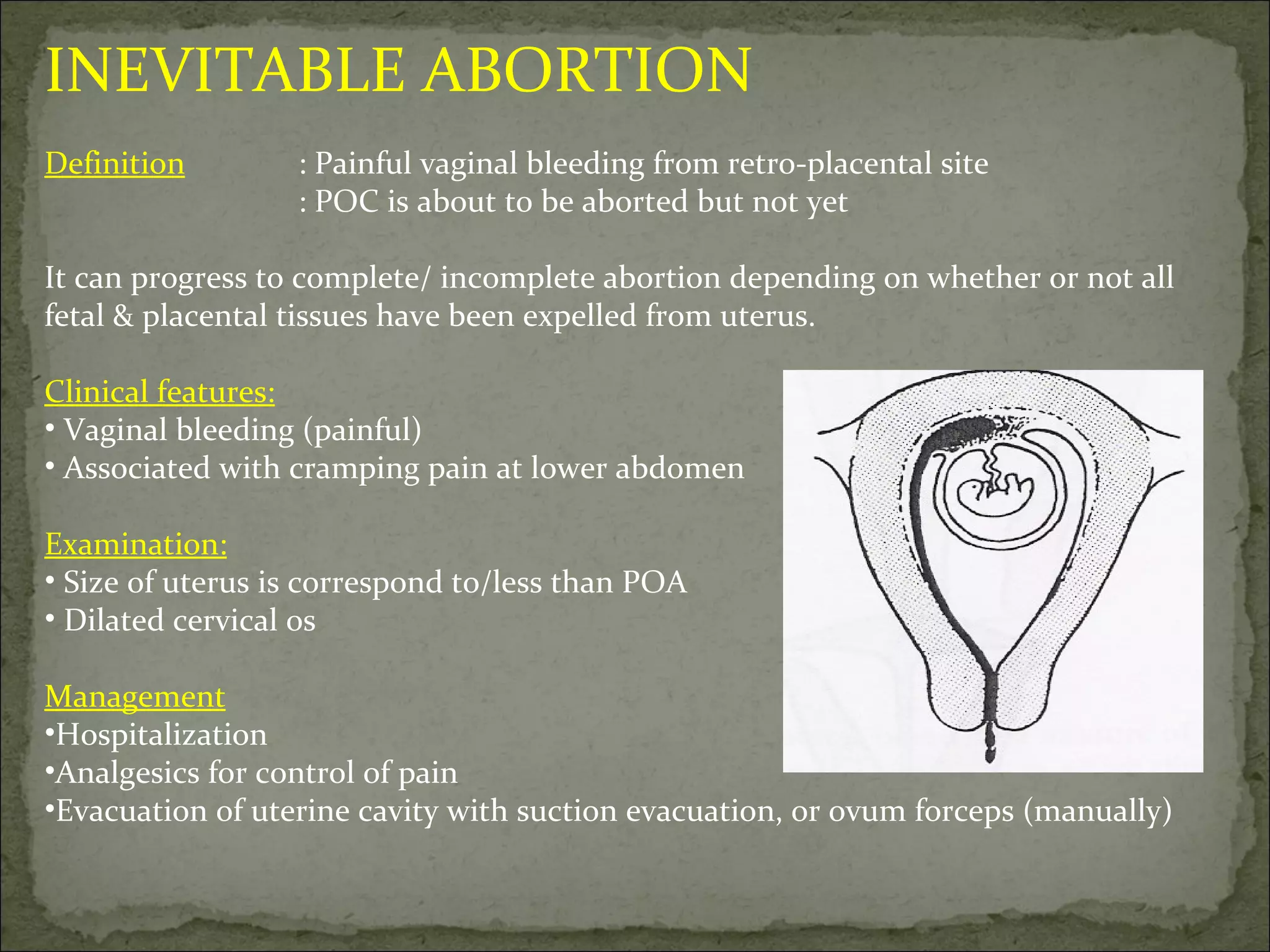
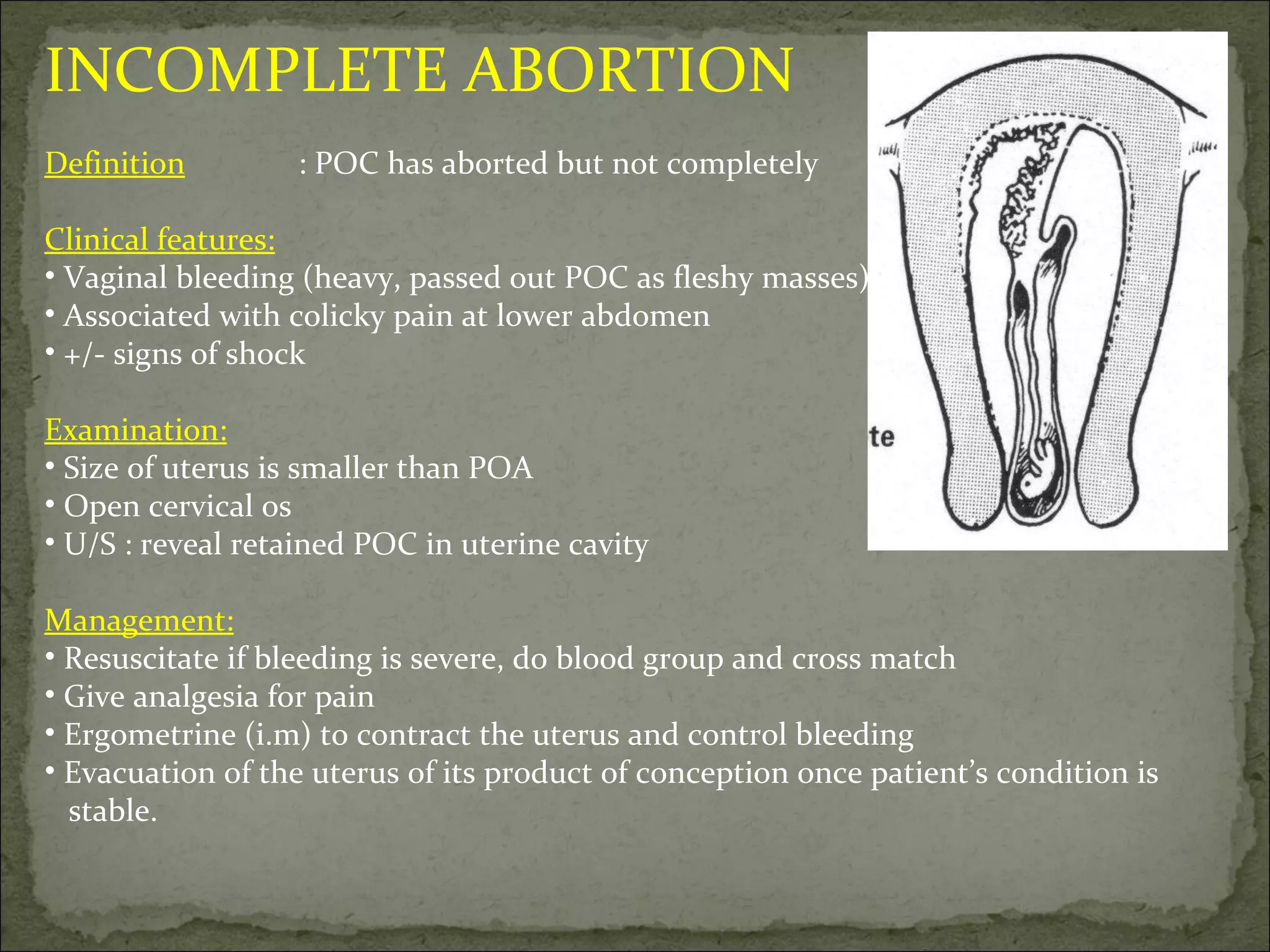
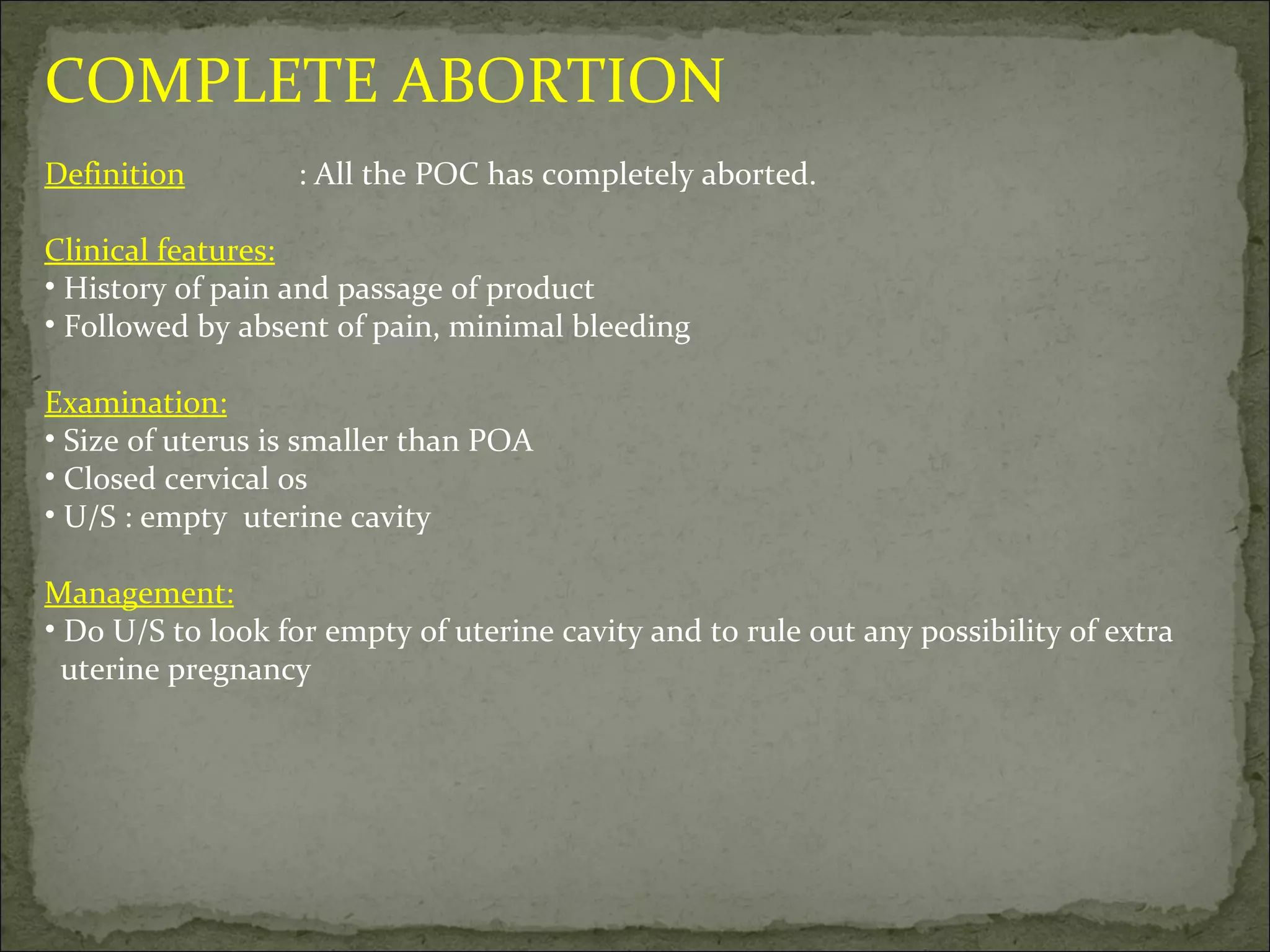
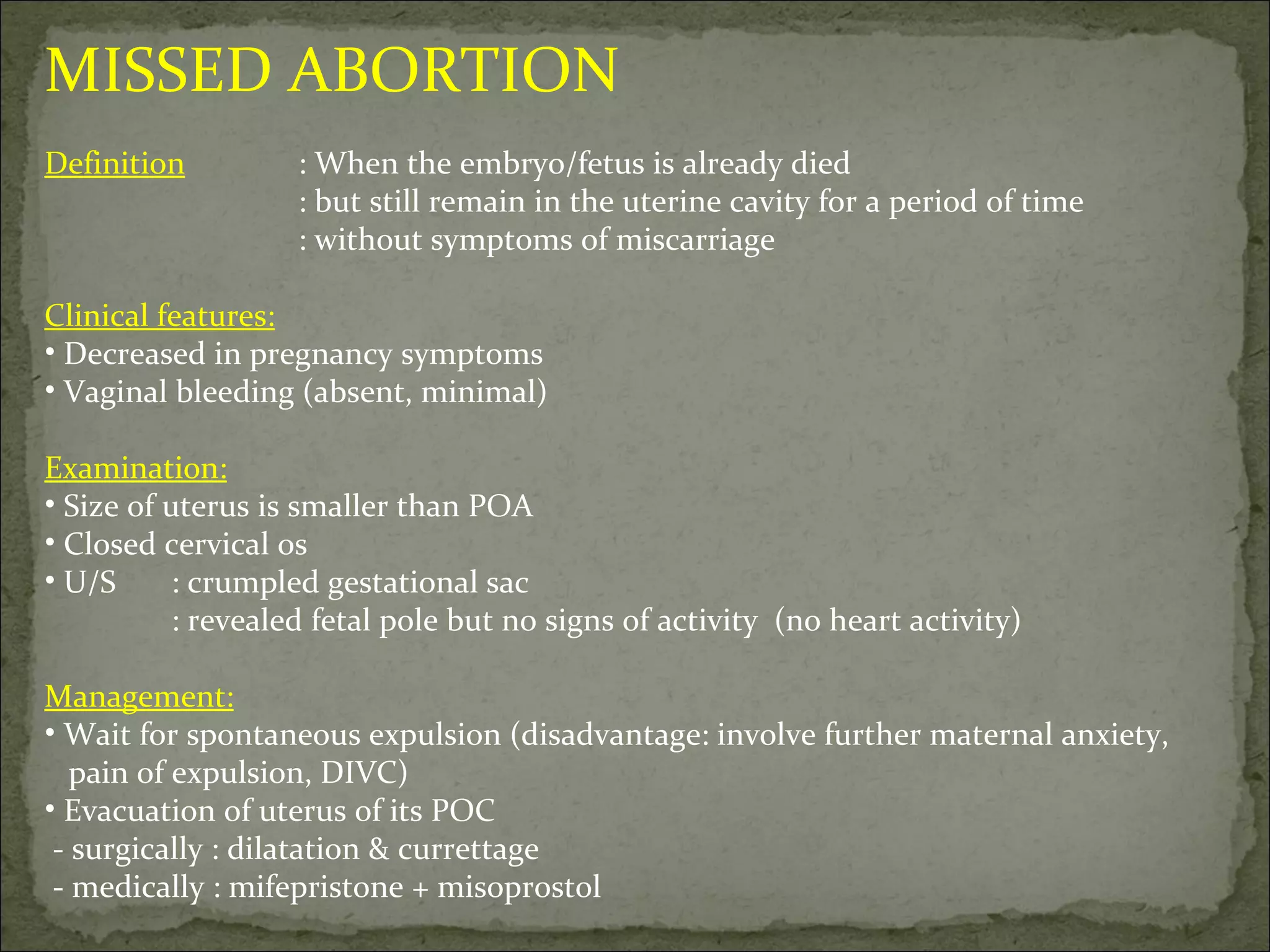
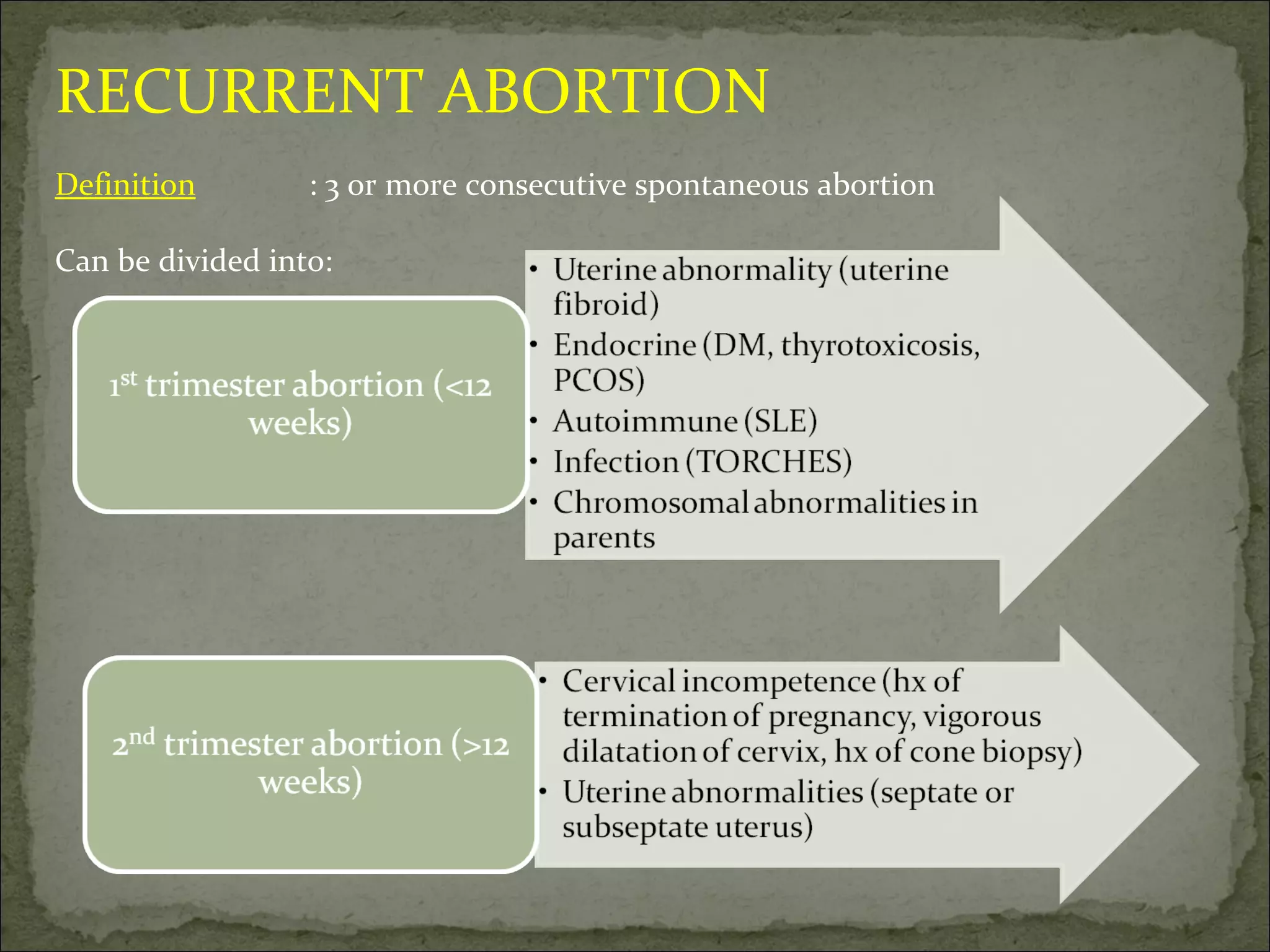
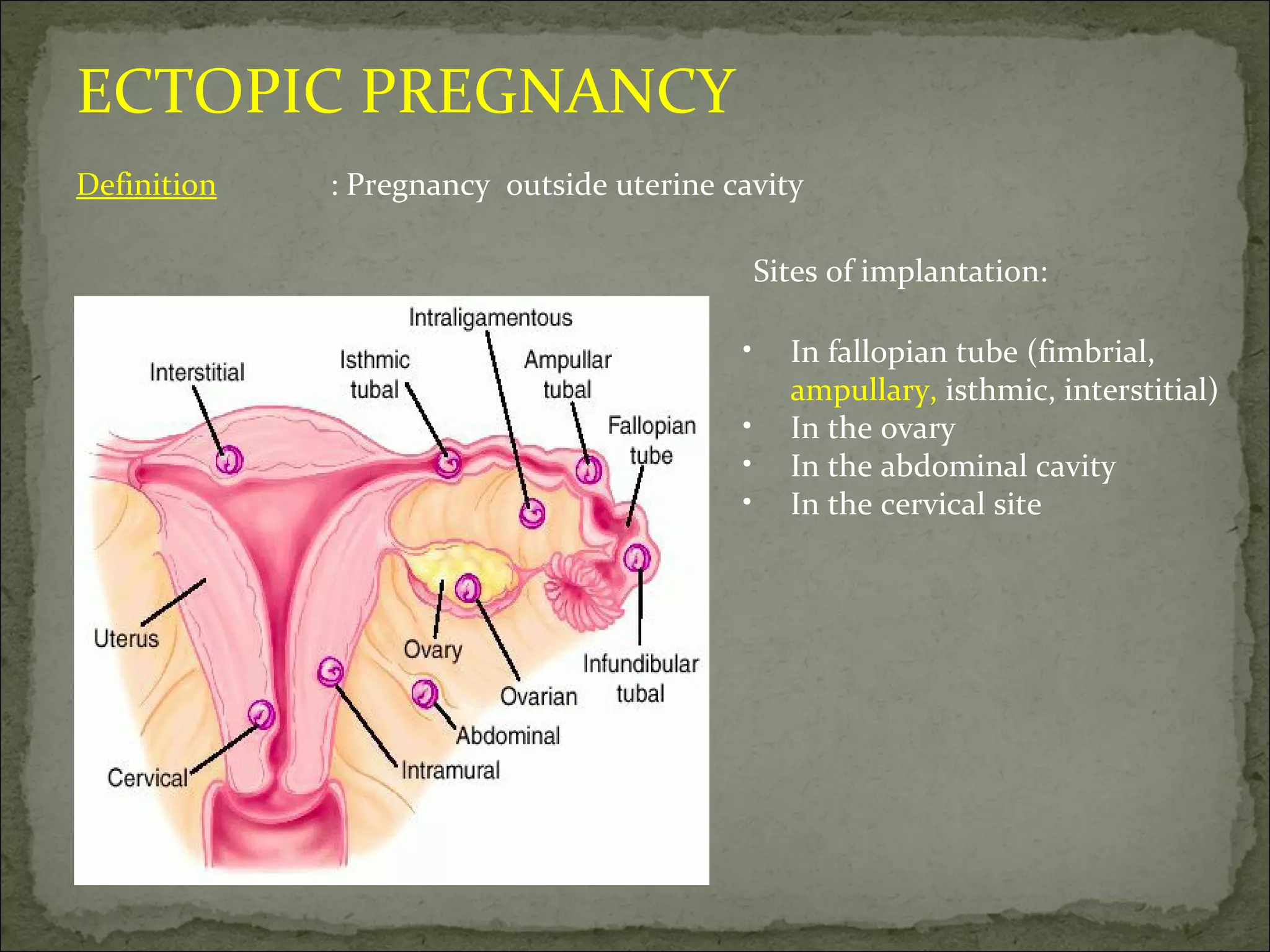
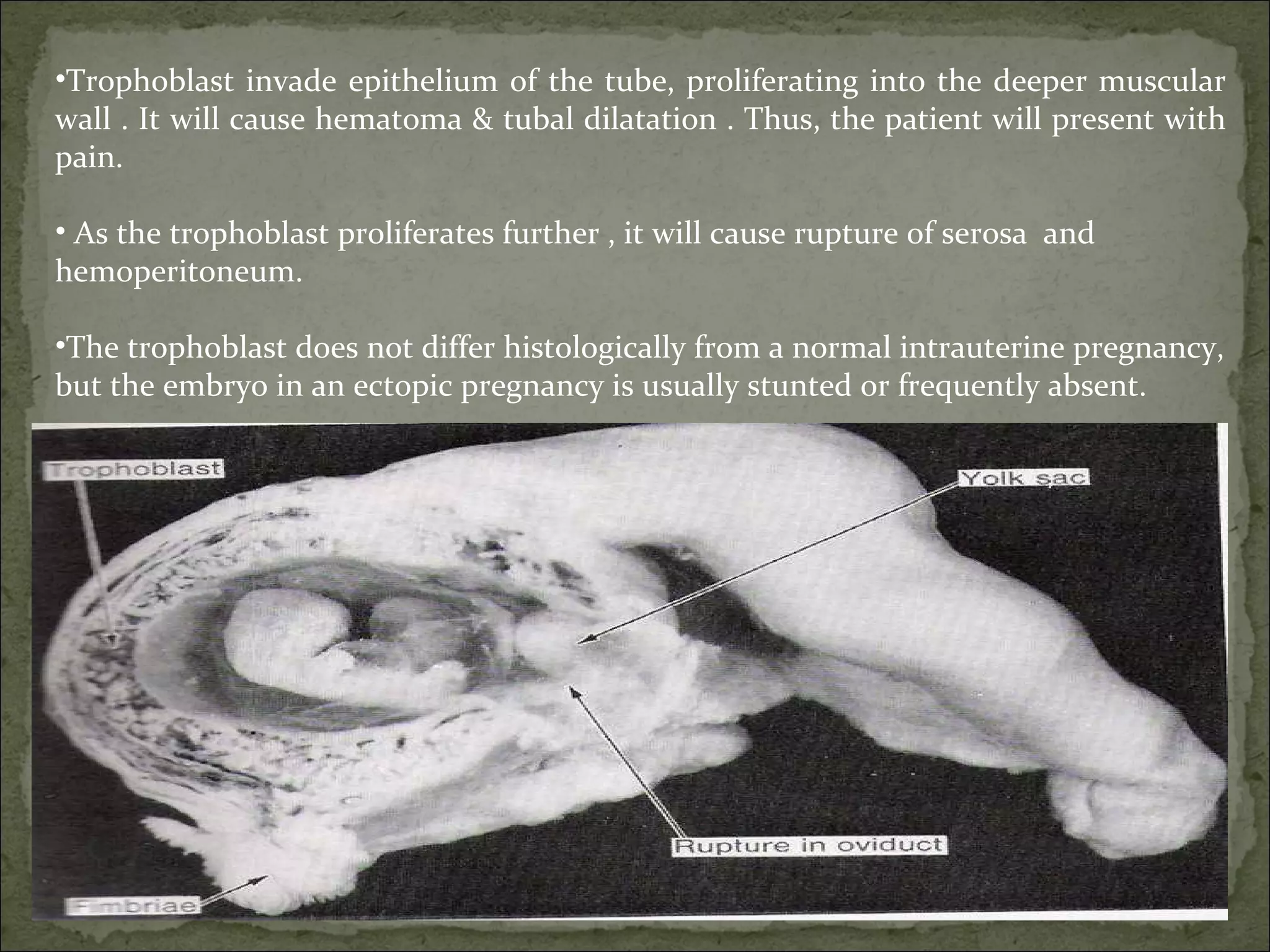
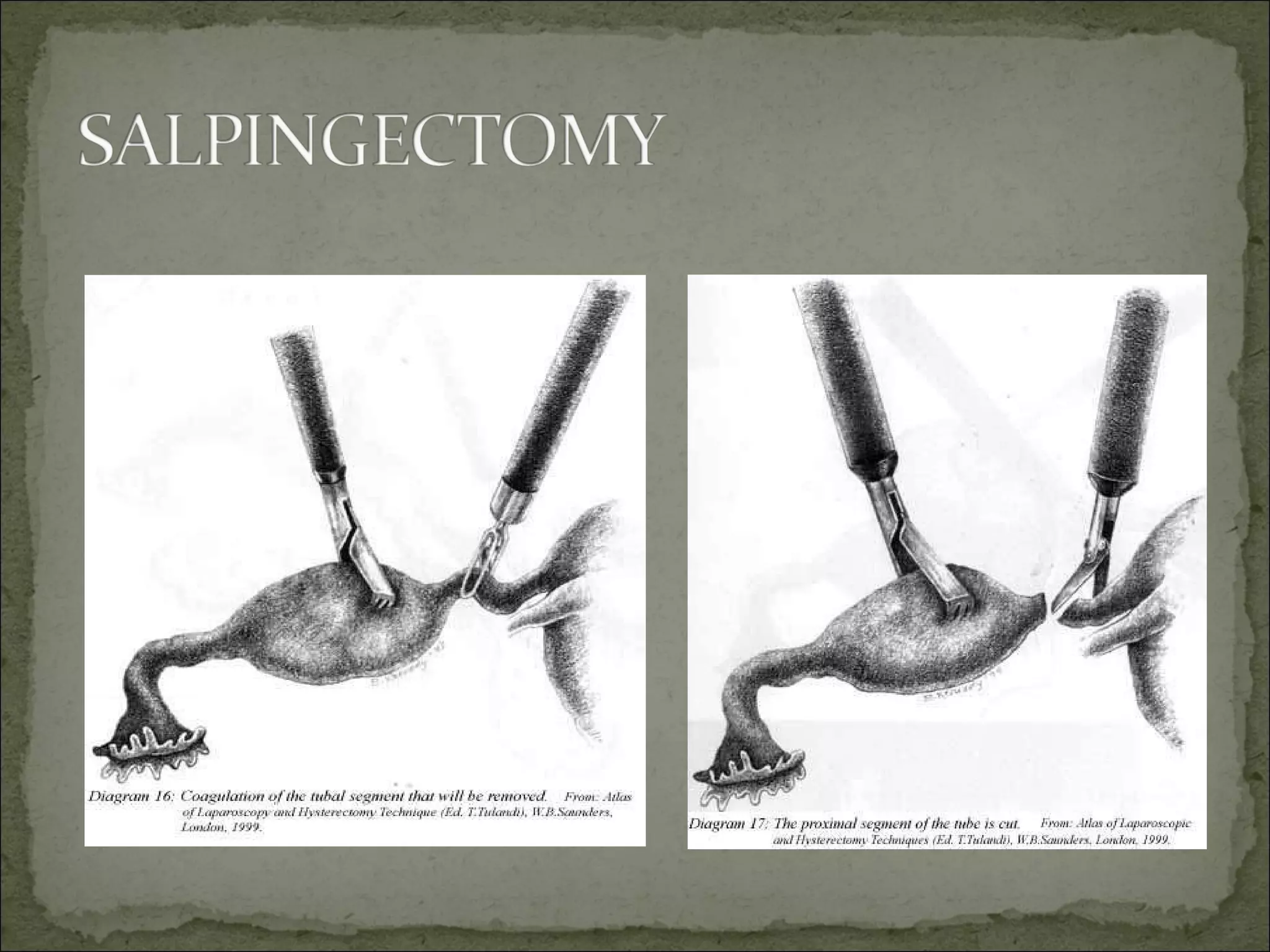
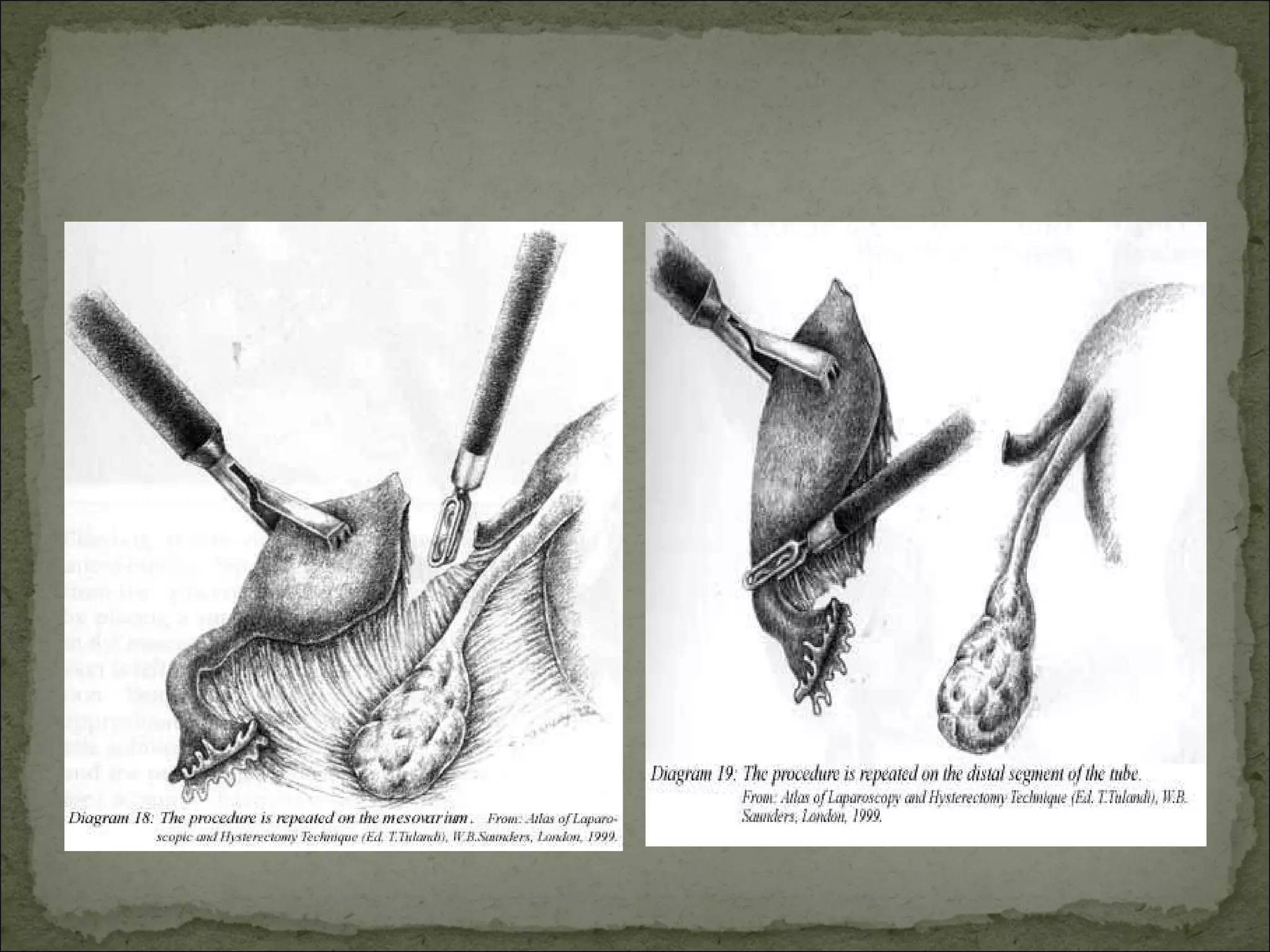
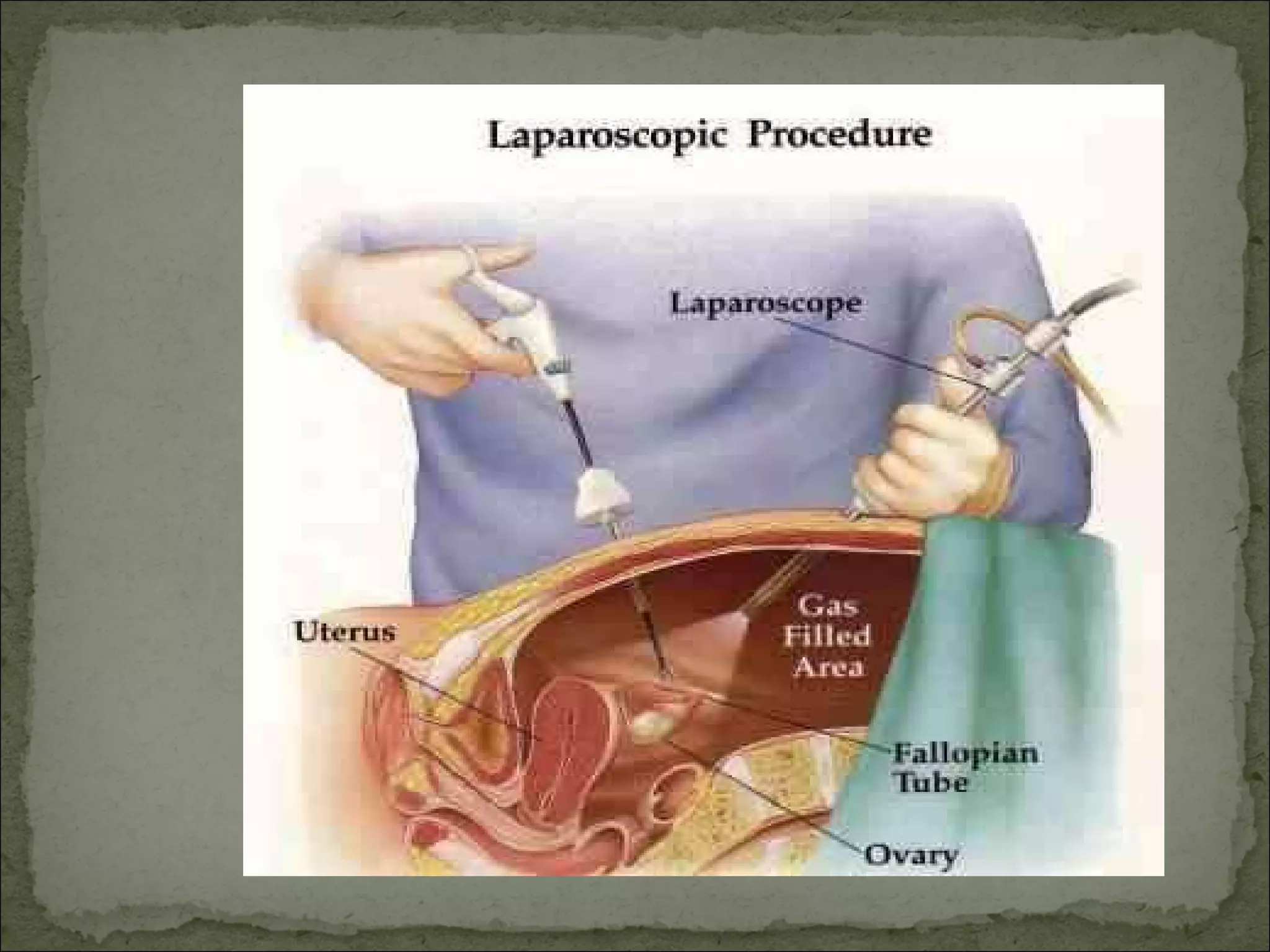
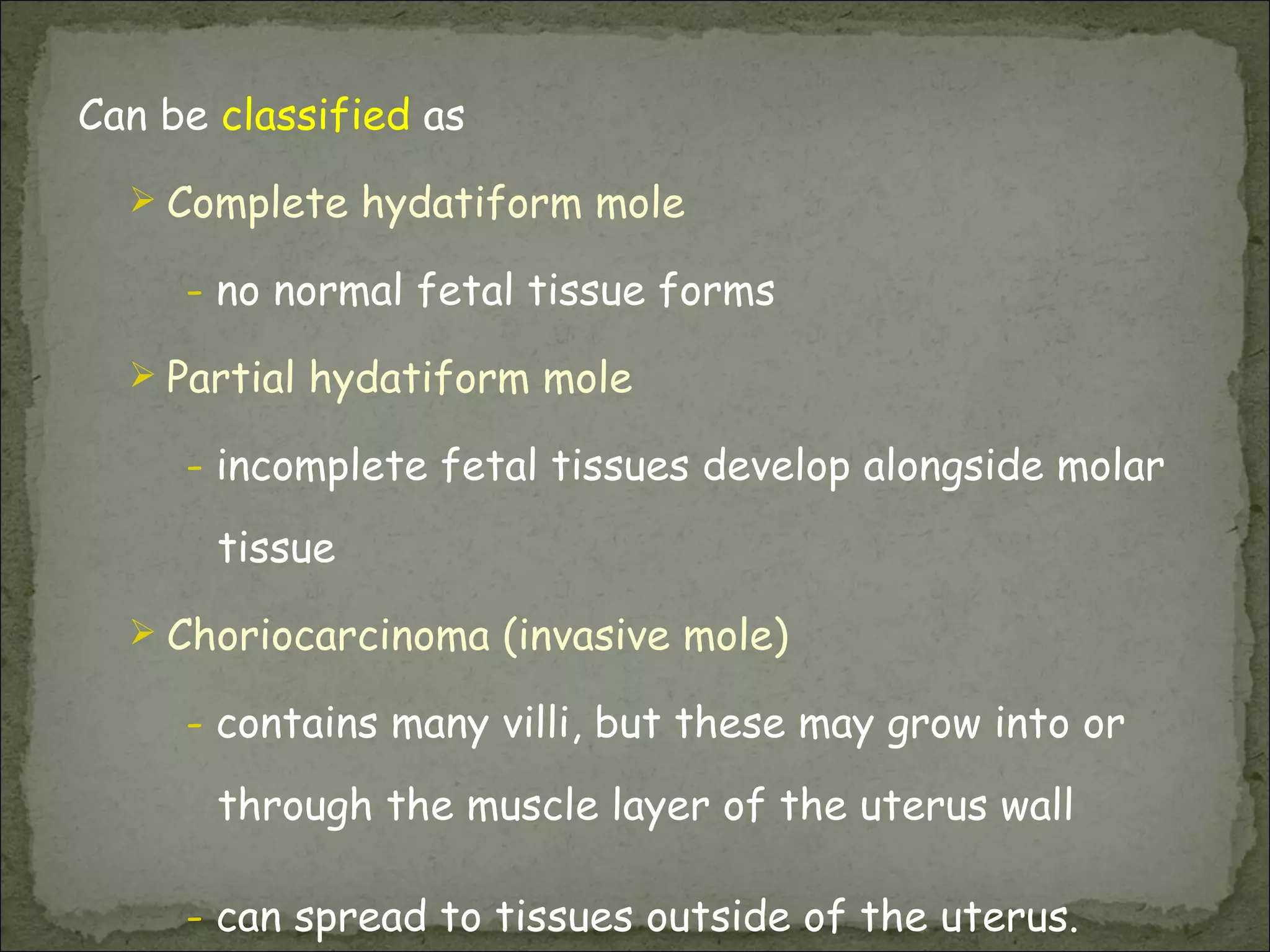
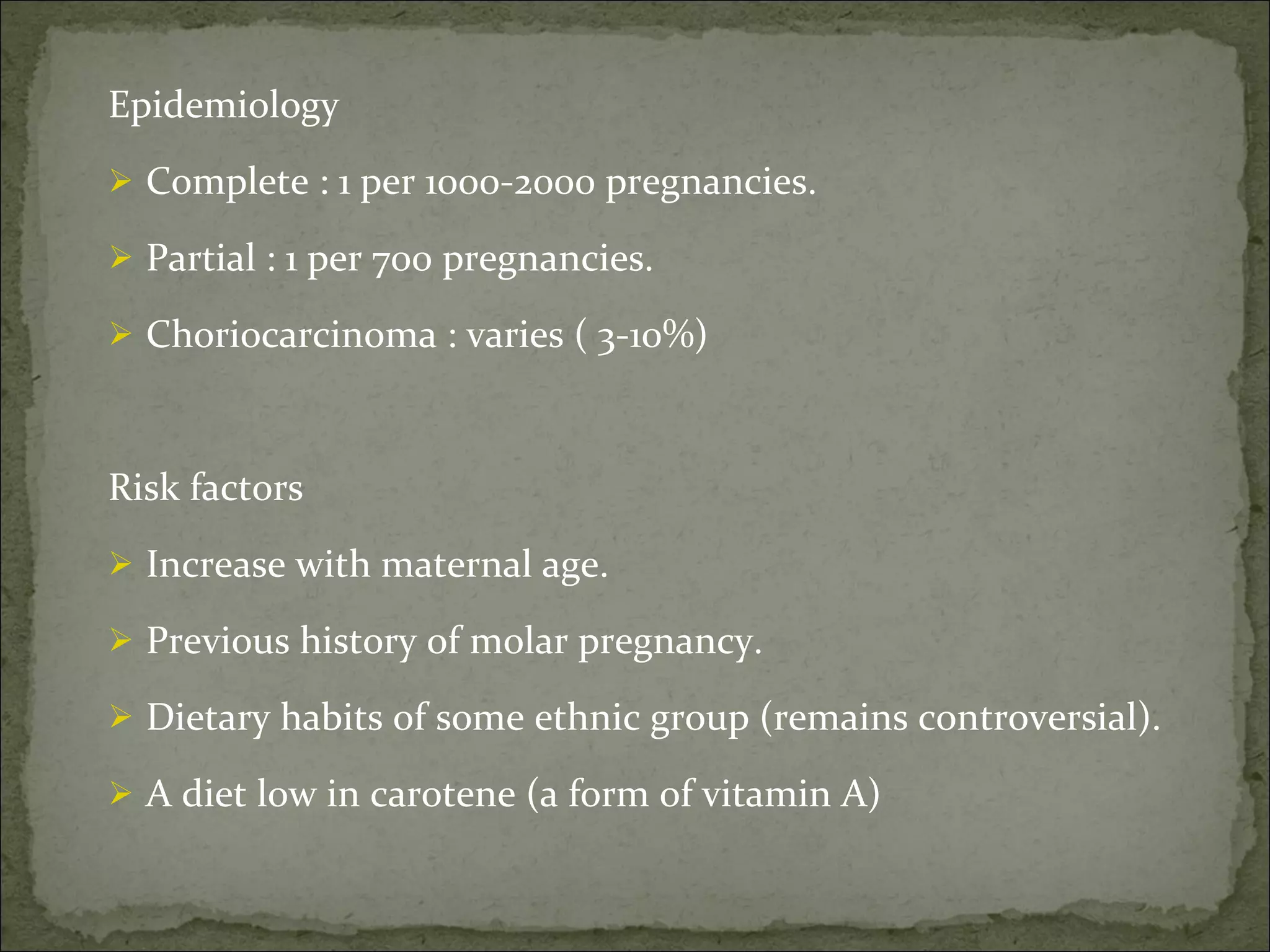
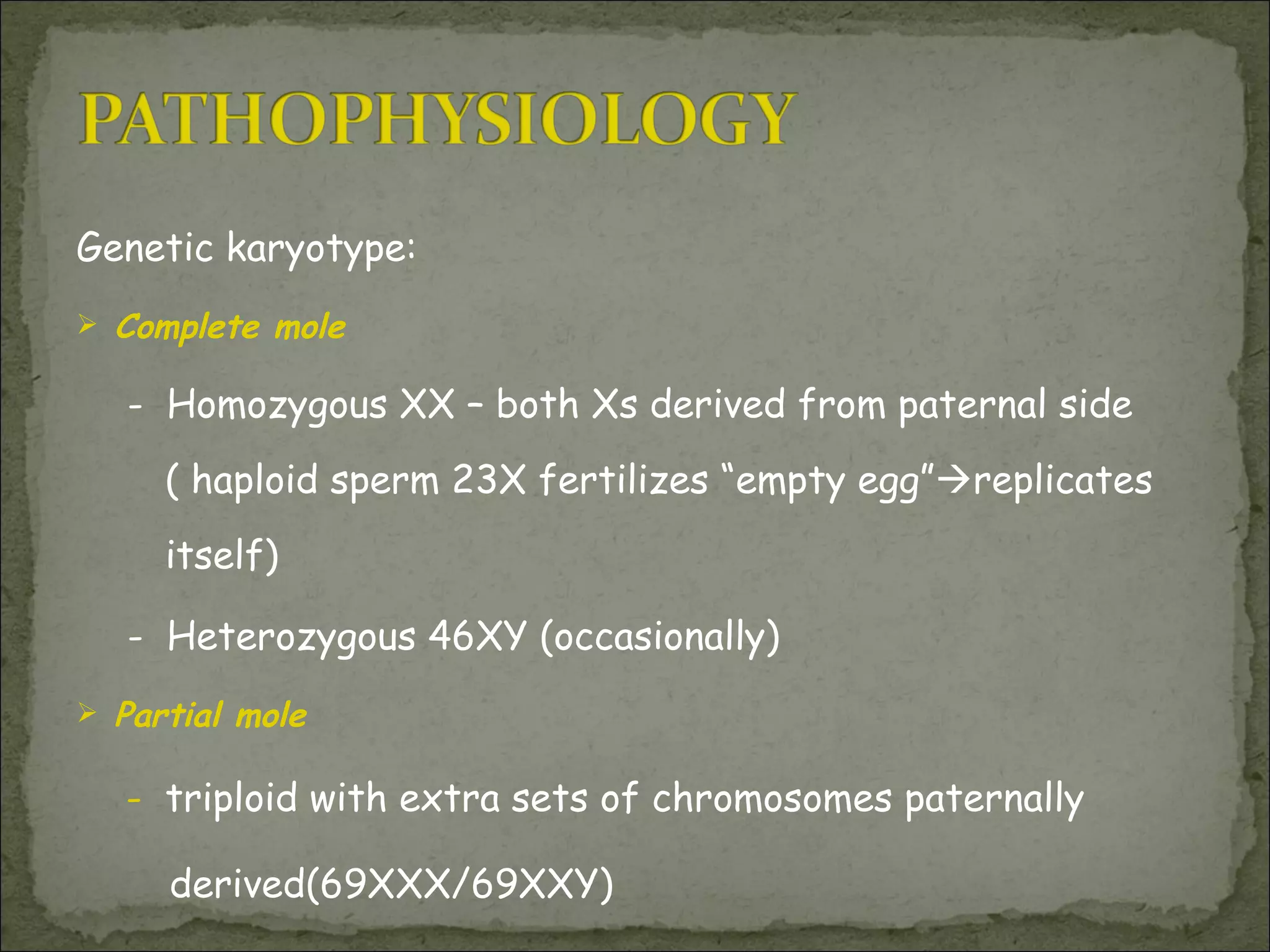
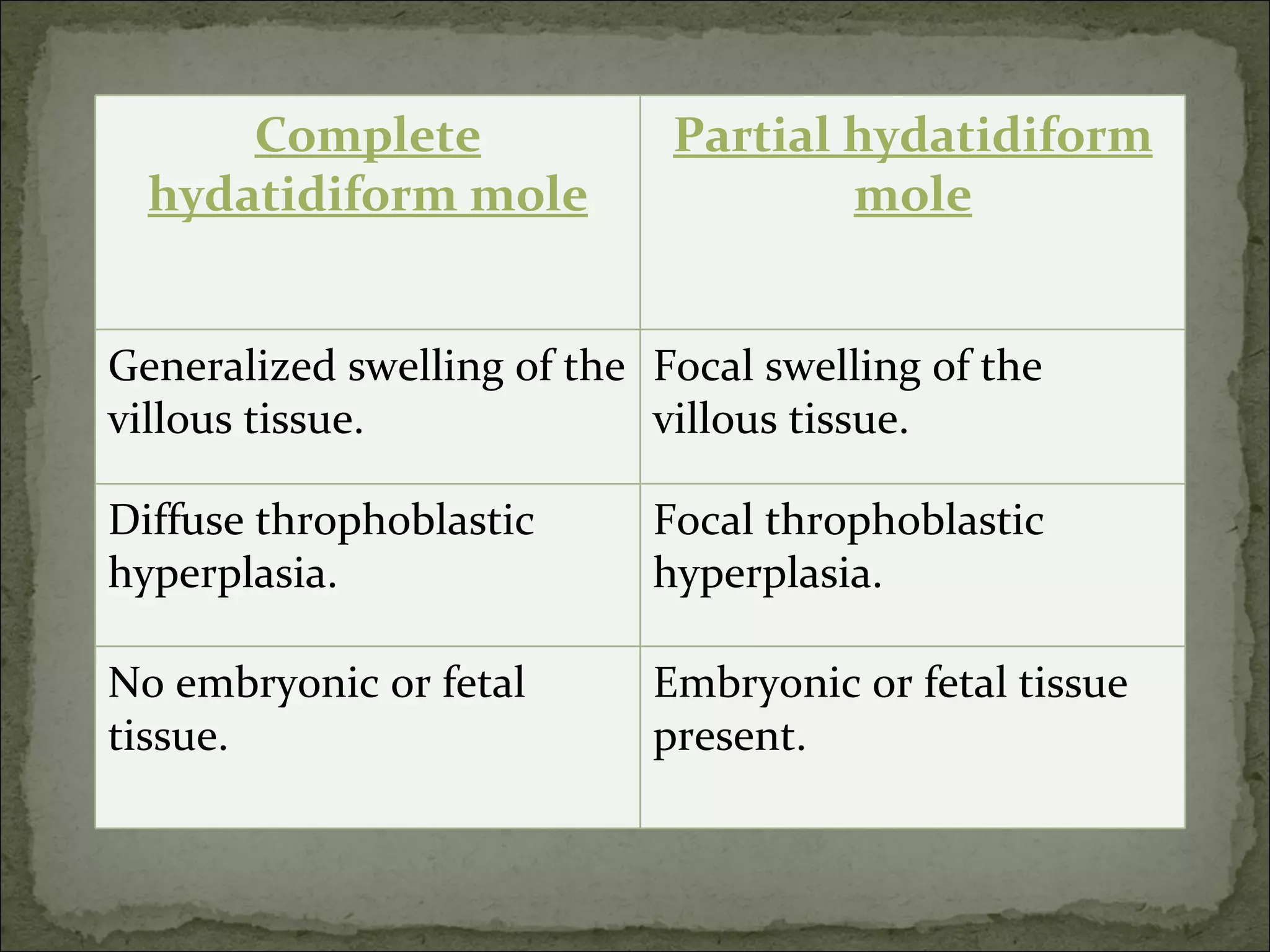
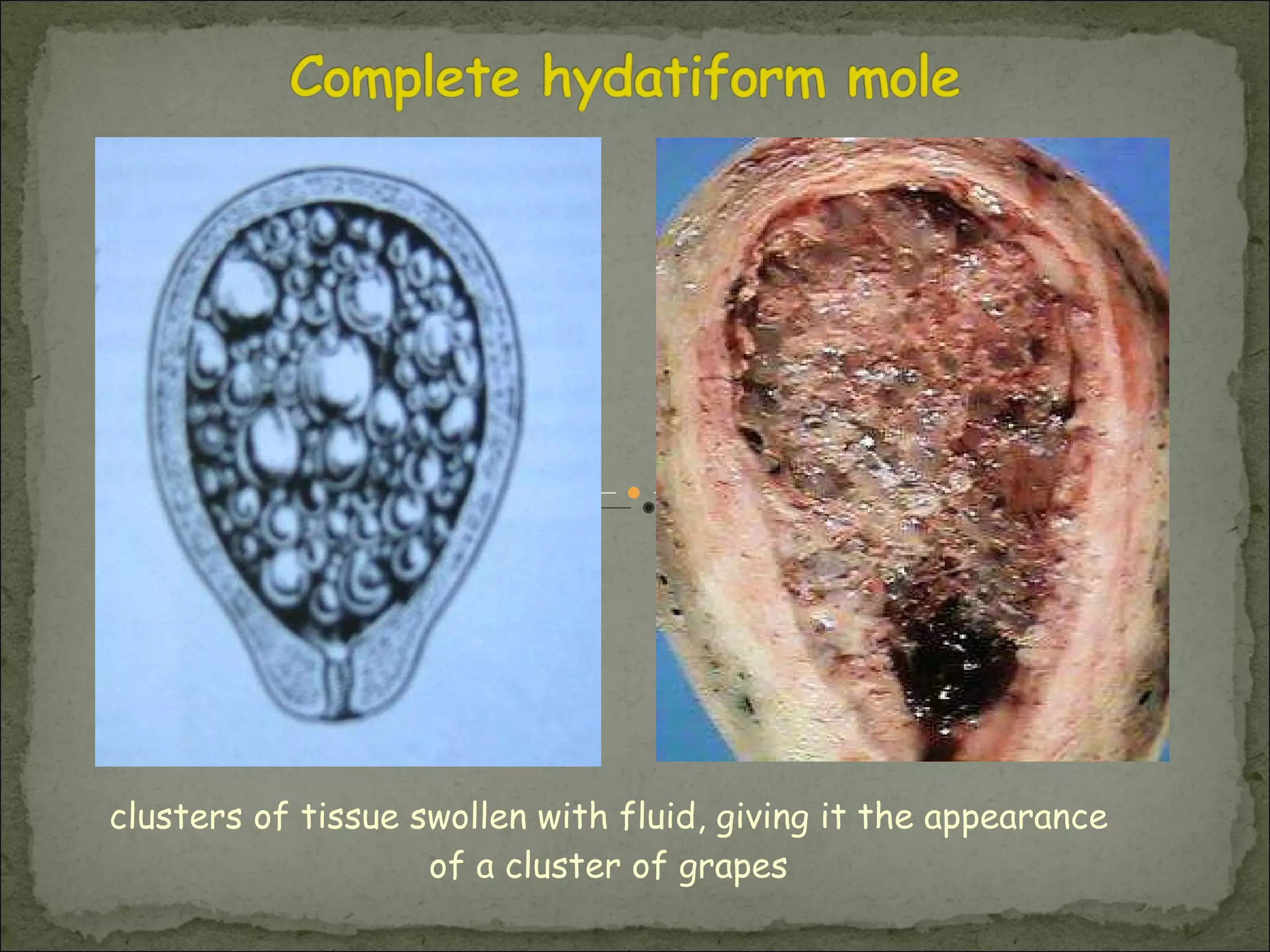
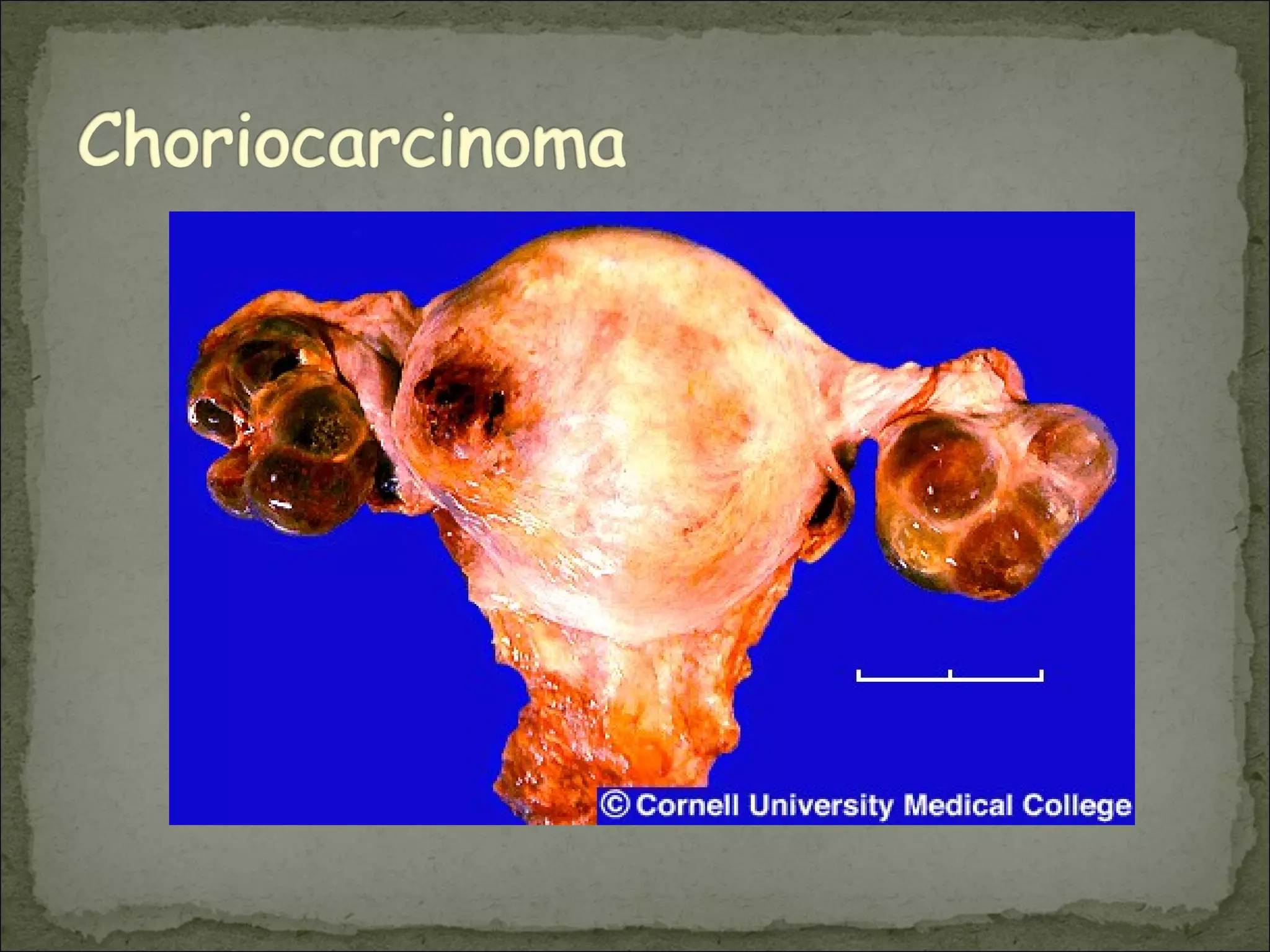
The three main categories of early pregnancy disorders are abortion, ectopic pregnancy, and gestational trophoblastic disease. Abortion can be threatened, inevitable, incomplete, complete, or missed depending on whether fetal and placental tissues have been expelled. Ectopic pregnancies occur outside the uterus, often in the fallopian tubes, and can cause pain and bleeding. Gestational trophoblastic disease includes complete and partial hydatidiform moles, as well as choriocarcinoma, and involves abnormal proliferation of trophoblast tissue.