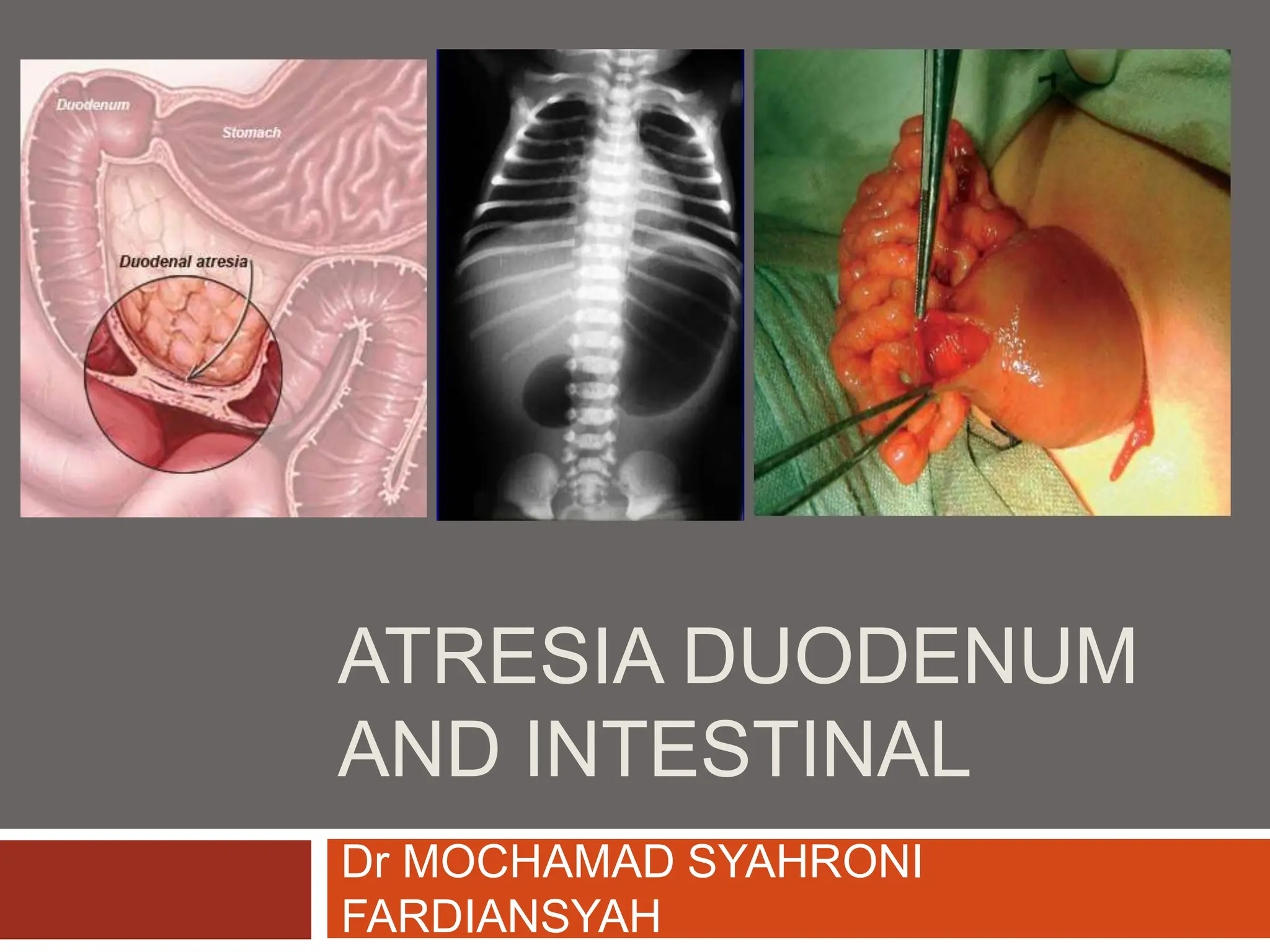
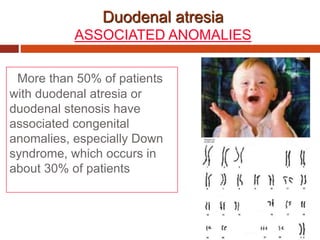
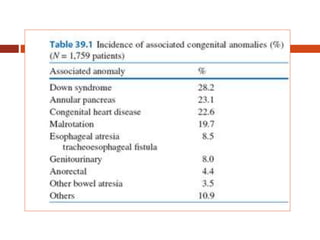
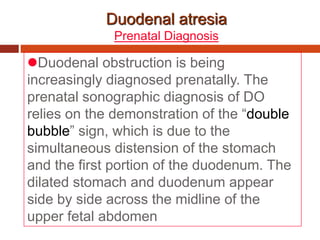
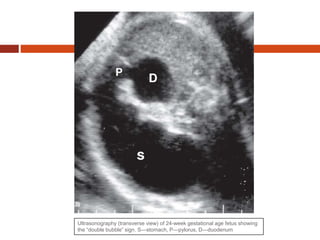
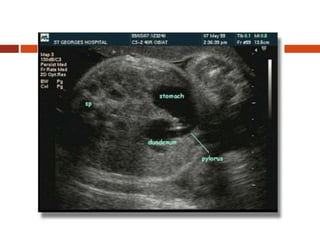
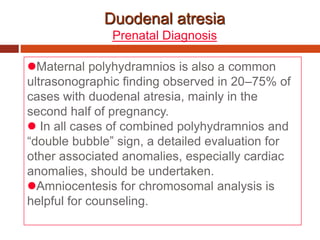
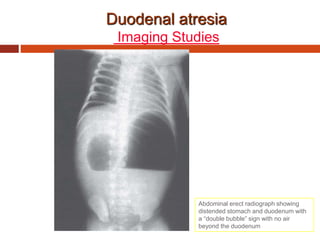
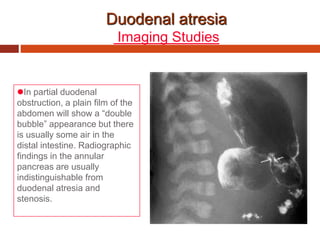
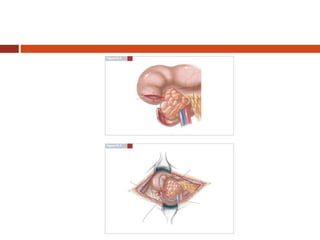
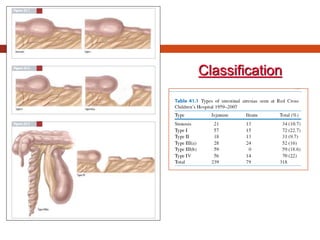
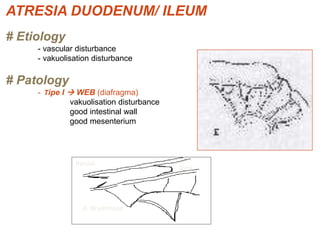
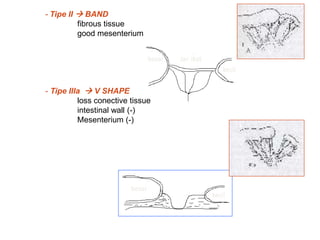
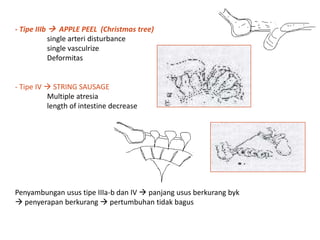
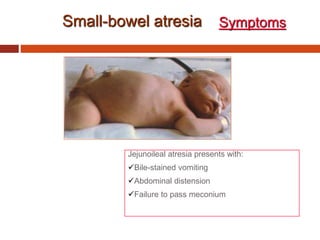
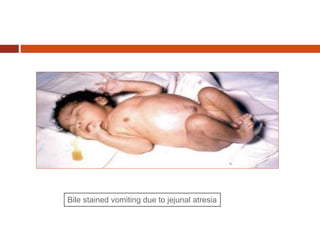
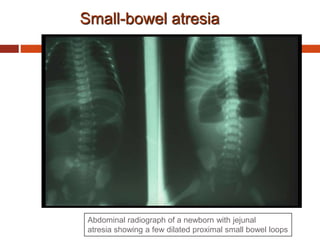
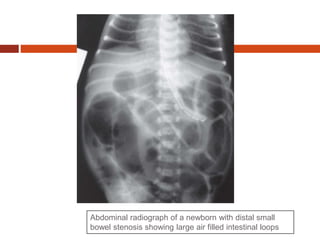
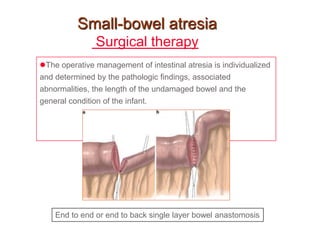
This document discusses duodenal atresia and intestinal atresia. It notes that duodenal atresia occurs in 1 in 5,000-10,000 births and is more common in boys. Over 50% of cases have associated anomalies like Down syndrome. Prenatal diagnosis is now possible using ultrasound to identify the "double bubble" sign of a dilated stomach and duodenum. Surgical repair typically involves a duodenoduodenostomy. Jejunoileal atresia has a prevalence of 1 in 330-1,500 births and also requires surgical repair typically using an end-to-end or end-to-back anastomosis.