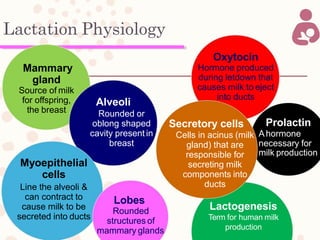
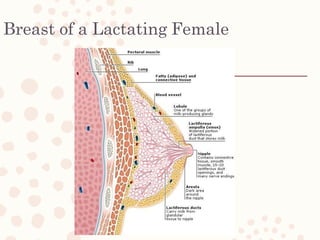
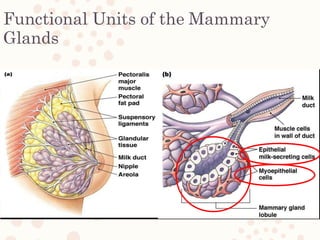
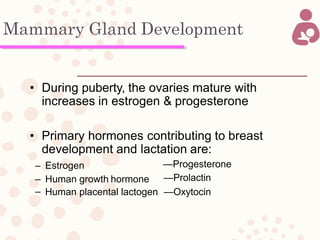
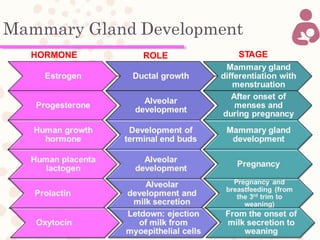
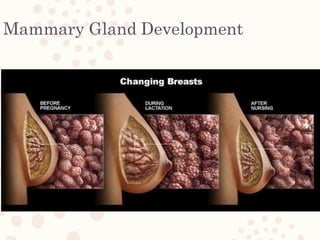
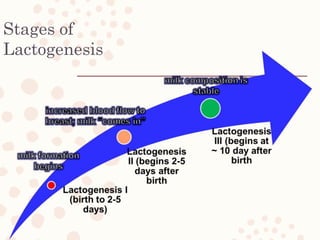
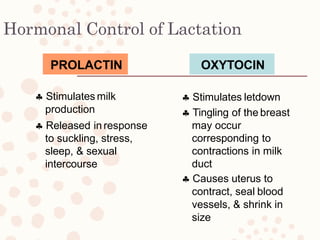
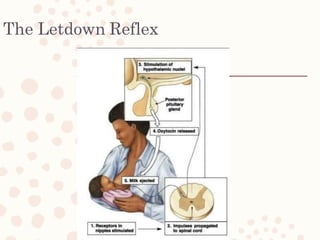
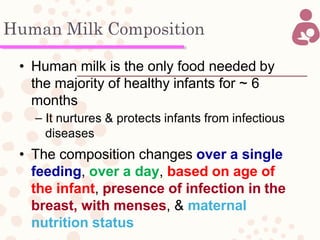
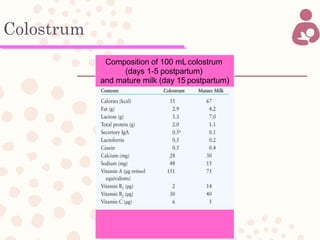
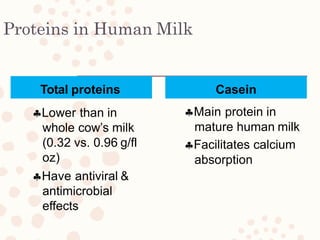
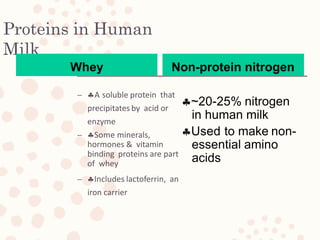
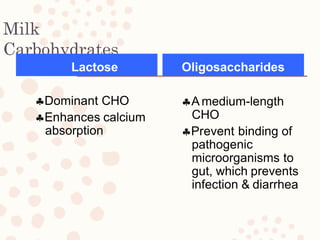
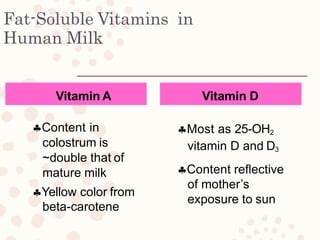
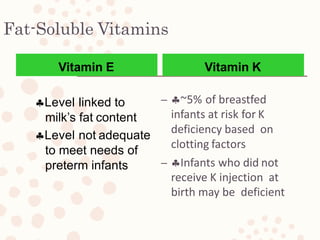
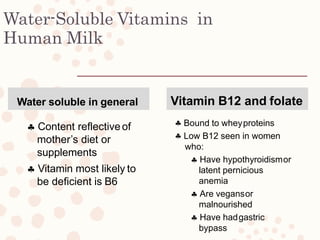
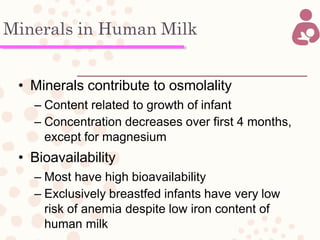
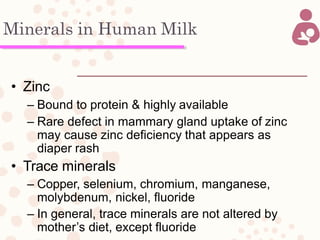
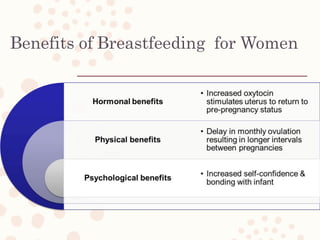
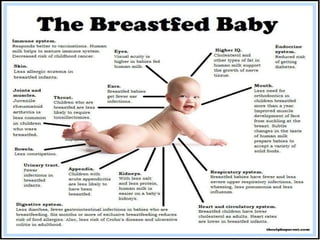
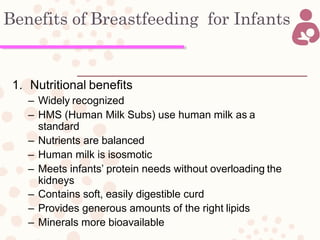
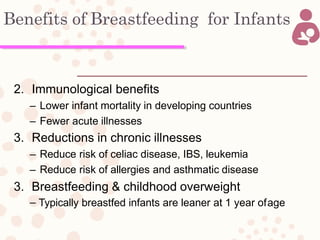
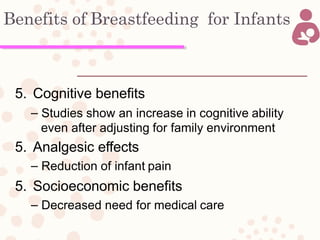
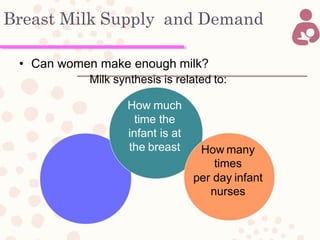
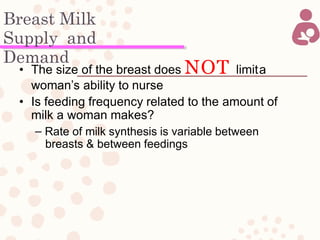
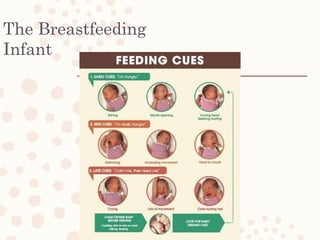
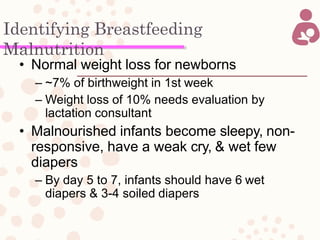
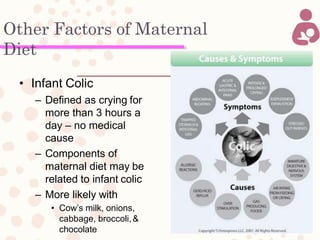
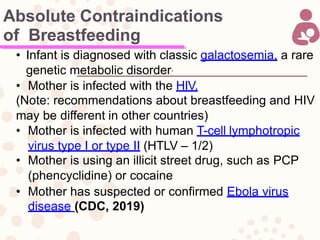
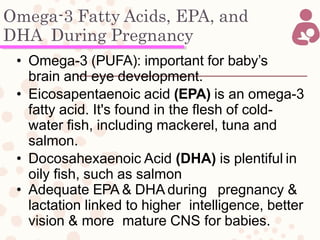
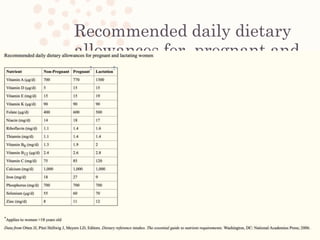
The document by Dr. M. Shoukri provides an extensive overview of breastfeeding and maternal nutrition, detailing lactation physiology, the composition of human milk, and the hormonal influences involved in lactation. It discusses the benefits of breastfeeding for both infants and mothers, the importance of maternal diet, and the factors affecting milk supply and demand. Additionally, the document addresses common breastfeeding challenges and the nutritional needs of lactating women.