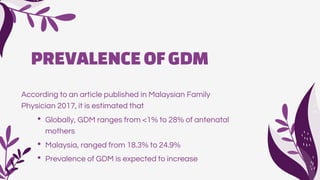
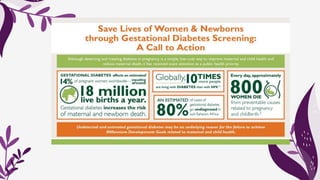
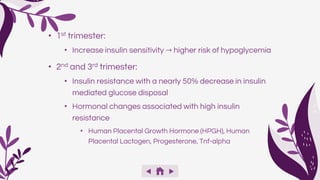
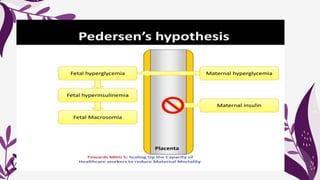
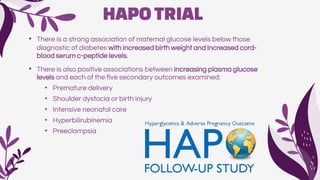
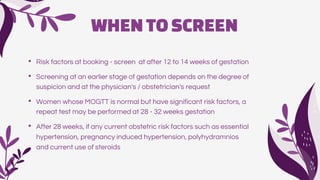
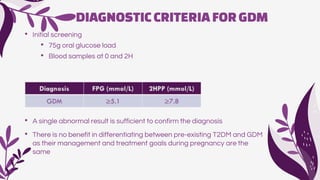
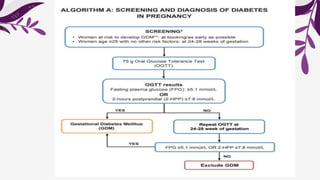
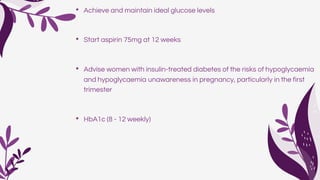
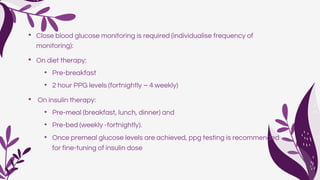
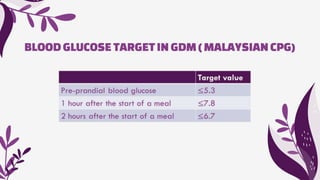
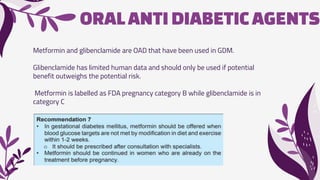
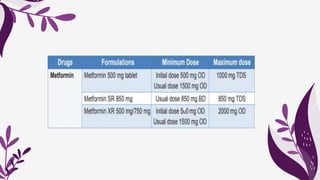
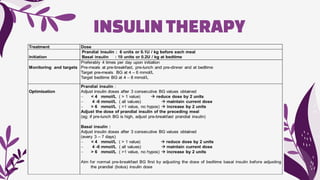
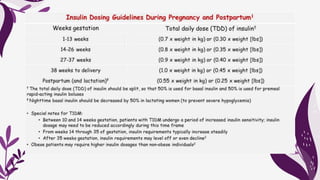
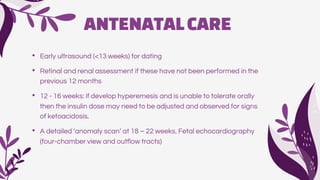
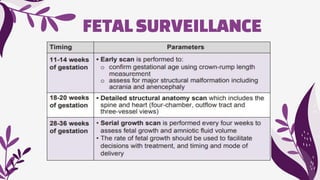
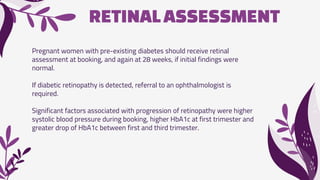
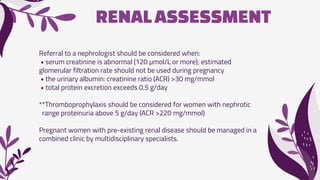
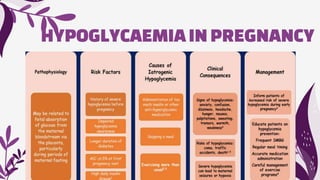
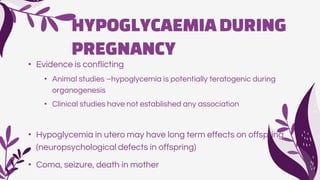
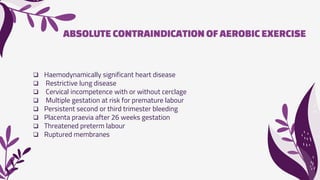
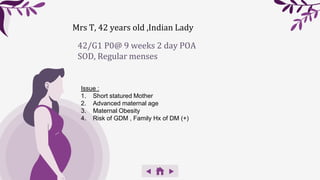
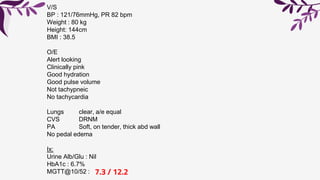
This document provides an overview of the management of gestational diabetes mellitus (GDM). It defines GDM and discusses its prevalence and pathophysiology. It outlines maternal and fetal complications of GDM. The document discusses screening, diagnostic criteria, and treatment targets for GDM. It also covers preconception counseling, antenatal care including monitoring, medical nutrition therapy, exercise recommendations, and fetal surveillance in the management of GDM.