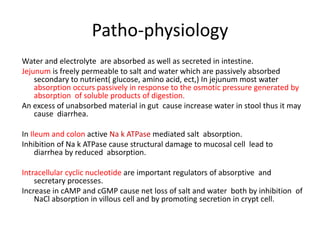
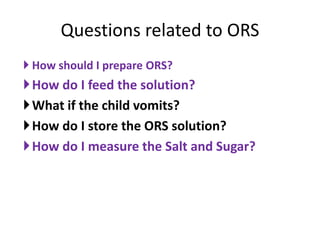
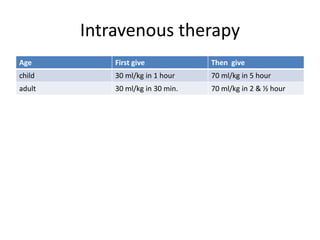
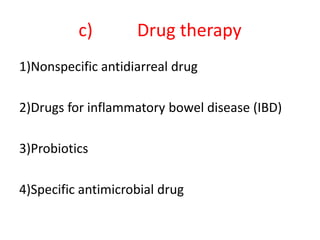
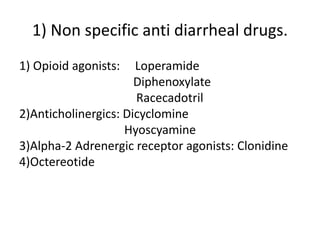
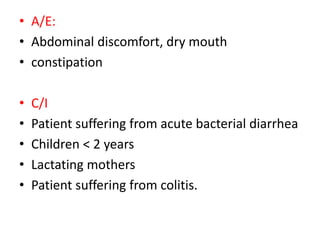
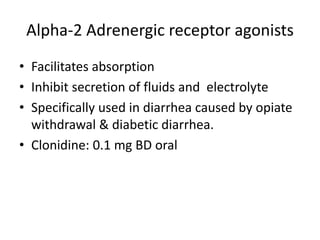
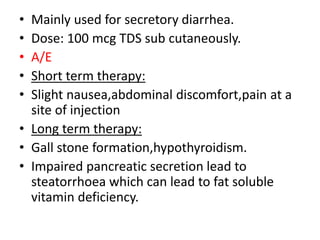
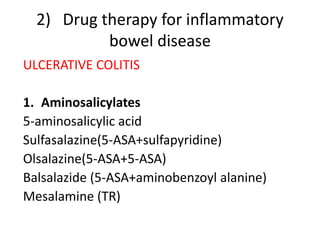
This document summarizes information about anti-diarrheal drugs. It defines diarrhea and describes its causes such as diet, infection, drugs, and stress. It classifies diarrhea as acute or chronic and discusses causes of infectious diarrhea. Treatment principles focus on rehydration therapy with oral or intravenous fluids. Specific anti-diarrheal drugs are discussed like opioids, anticholinergics, alpha-2 adrenergic agonists, and octreotide. Management of inflammatory bowel diseases with drugs targeting TNF-alpha and immunosuppressants is also covered. The role of probiotics and specific antimicrobial drugs for different infections is summarized.