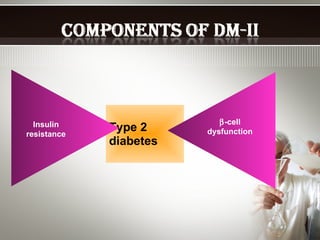
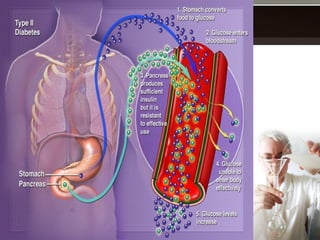
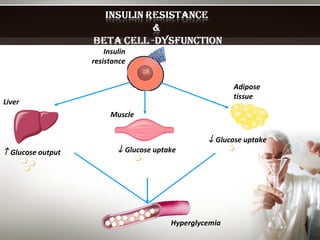
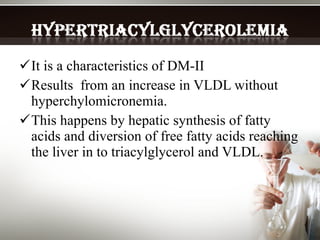
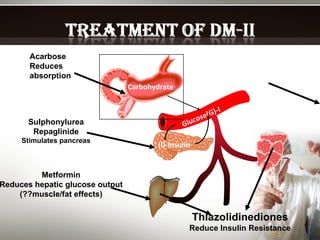
- Type 2 diabetes is characterized by insulin resistance, inadequate insulin secretion from the pancreas, and elevated blood glucose levels. This can lead to complications affecting small blood vessels (microvascular), large blood vessels (macrovascular), and nerves (neuropathic).
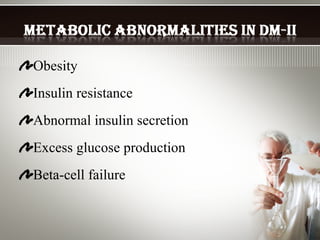
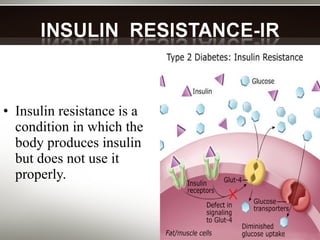
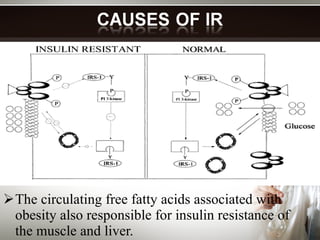
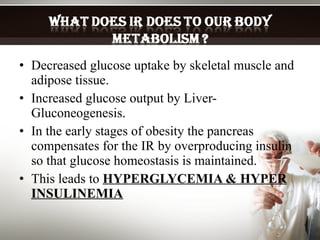
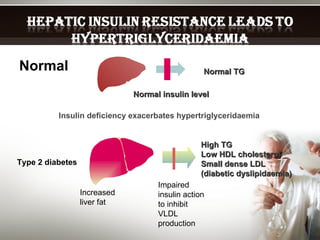
- Insulin resistance develops when the body does not properly use insulin and is associated with obesity. Over time, this can cause the pancreas to lose its ability to produce enough insulin to compensate, leading to high blood glucose and insulin levels.
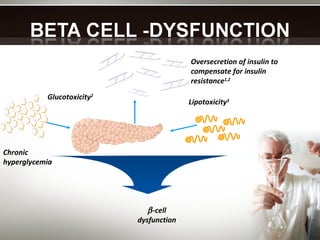
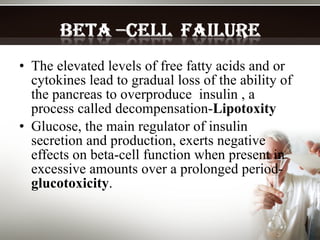
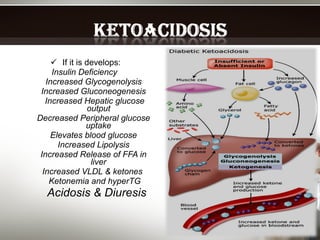
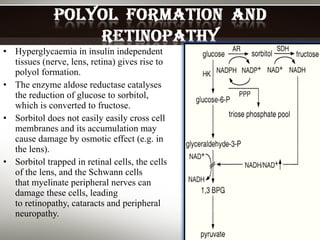
- Chronic high blood glucose can damage tissues and cells in the body through processes like glucotoxicity and lipotoxicity, worsening insulin resistance and beta cell function over time in a vicious cycle. This puts individuals at higher risk for