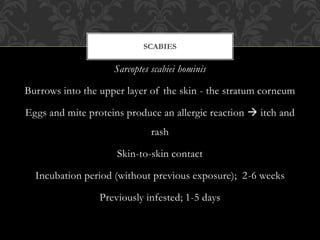
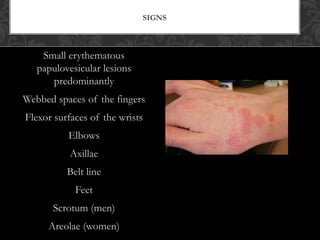
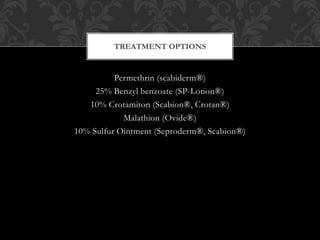
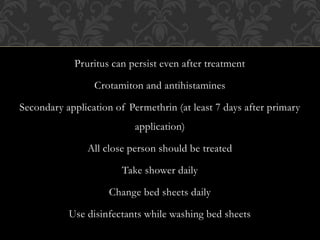
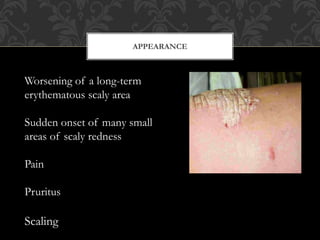
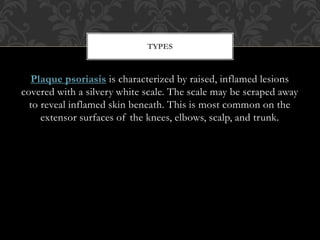
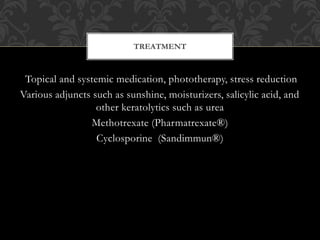
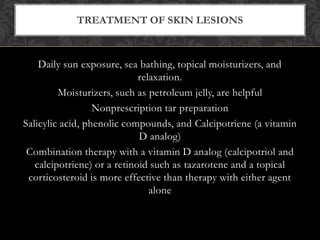
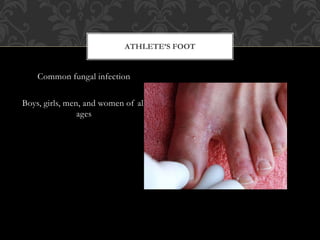
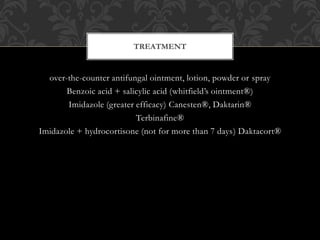
Sarcoptes scabiei causes scabies, presenting as itchy rash and small burrows in the skin. Symptoms include intense itching worse at night. Permethrin and benzyl benzoate are used for treatment. Psoriasis is a chronic, inflammatory skin condition causing red, scaly plaques, especially on elbows and knees. Treatment includes topical medications and phototherapy. Athlete's foot is a fungal infection of the feet causing scaling and itching between the toes. Keeping feet dry and using antifungal medications or creams can treat it.