This document provides information on several common pediatric skin disorders:
- Atopic eczema is a chronic, inflammatory skin condition characterized by an itchy red rash that favors skin creases. Its cause involves genetic and environmental factors.
- Seborrheic dermatitis causes flaky, greasy, red rashes in areas with many oil glands. Its cause may involve skin yeasts but it is not contagious.
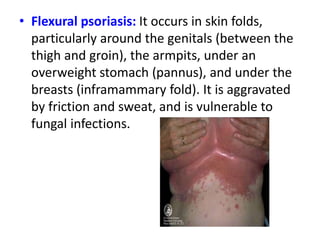
- Psoriasis causes raised red patches and silvery scales, and has genetic and environmental triggers. It has several clinical forms that vary in appearance and location on the body.