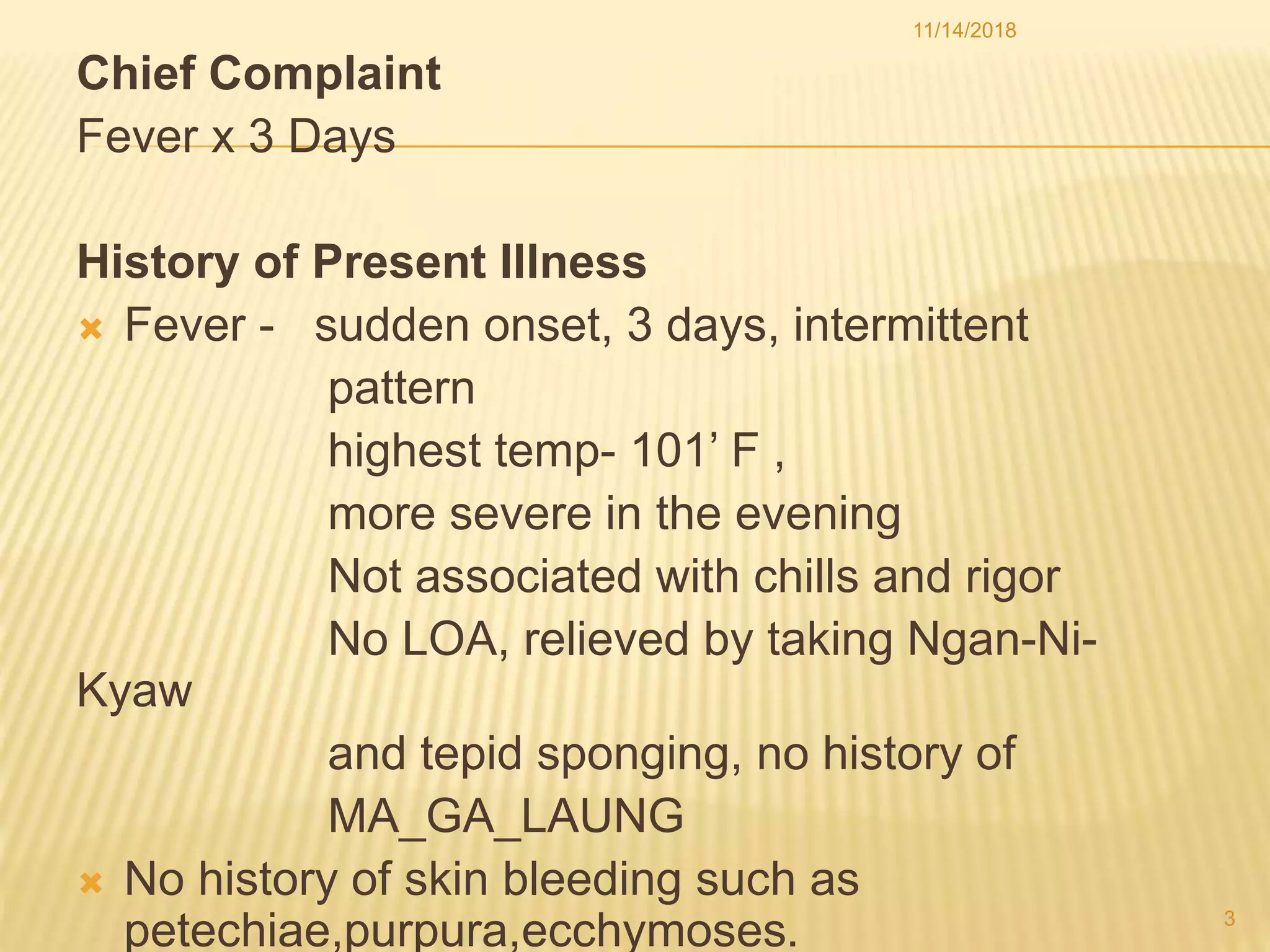
This document presents the case of a 4-year-old girl diagnosed with Dengue Hemorrhagic Fever Grade I. She presented with a 3-day history of intermittent fever up to 101°F. On examination, she displayed no signs of bleeding, shock, or complications. Her environment had many mosquito breeding grounds and lacked preventative measures. The provisional diagnosis was Dengue Hemorrhagic Fever Grade I based on her symptoms, positive Hess test, and relevant exposure history. She was treated with IV and oral fluids, paracetamol, and cetrine. Prevention strategies were discussed at the individual, family, community, and national levels focusing on environmental sanitation, mosquito netting