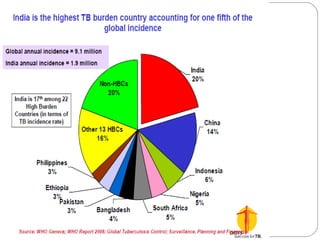
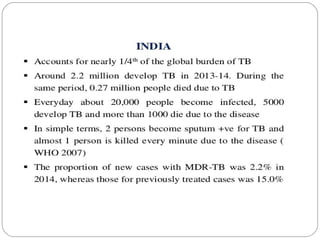
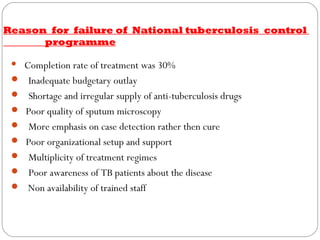
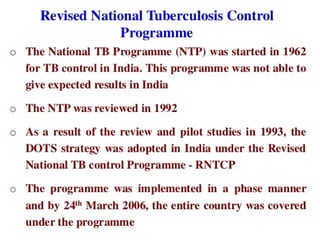
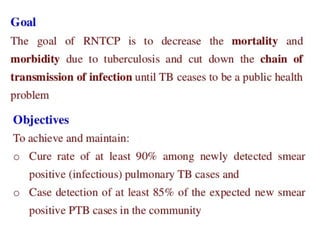
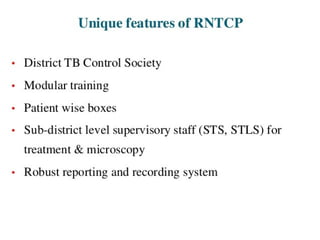
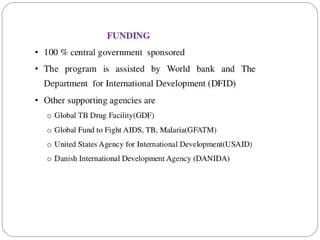
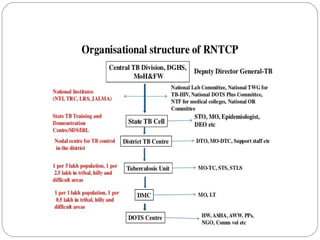
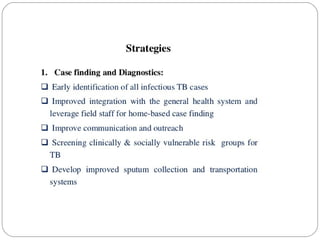
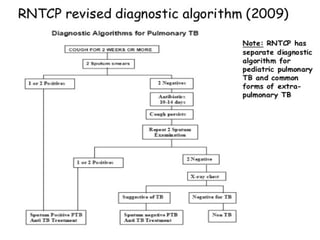
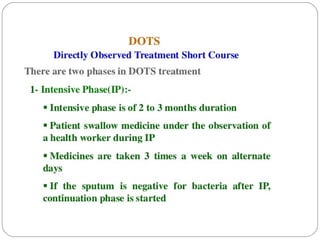
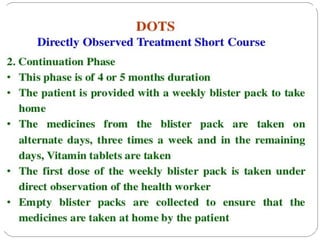
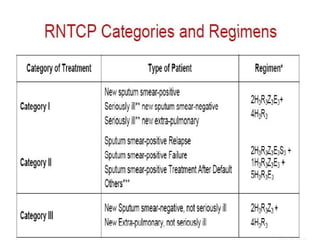
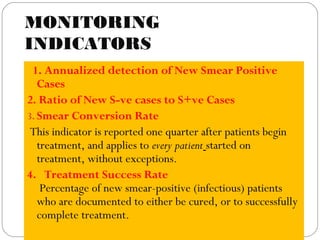
This document outlines the Revised National Tuberculosis Control Programme (RNTCP) in India. It summarizes that tuberculosis poses a major public health burden in India, accounting for 1/3rd of global cases. The National Tuberculosis Control Programme started in 1962, but failed due to low treatment completion rates and organizational issues. RNTCP was launched in 1997 with DOTS strategy, which involves directly observed treatment, short-course. RNTCP aims to reduce morbidity, mortality, and transmission of TB in India through early case detection and standardized treatment. It utilizes a decentralized organizational structure and relies on community health workers to observe treatment. If fully implemented, RNTCP aims to achieve global targets for TB control by improving cure rates and case