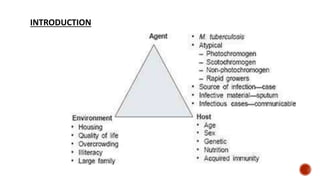
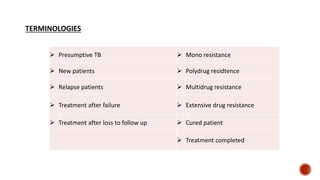
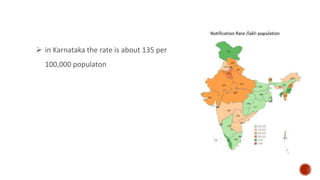
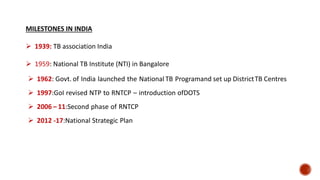
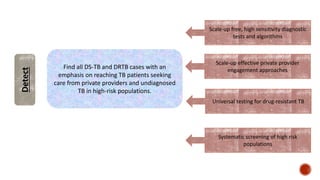
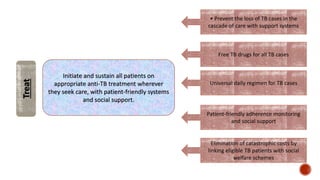
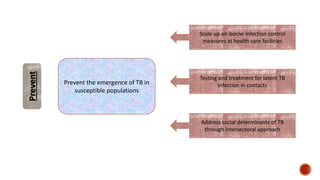
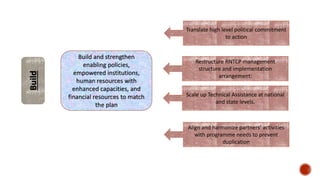
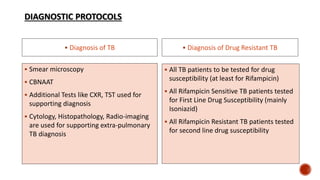
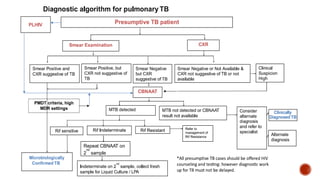
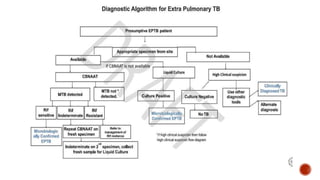
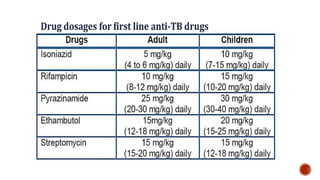
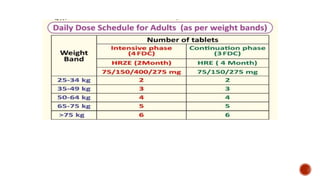
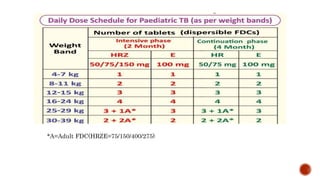
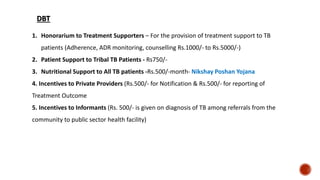
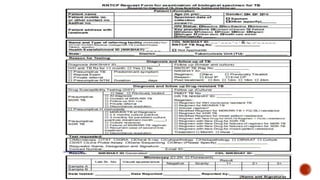
The document provides an overview of tuberculosis (TB) in India, including key terminology, disease burden statistics, milestones in the country's TB program, and details of the current National Tuberculosis Elimination Program (NTEP). It notes that India accounts for over a quarter of global TB cases. The NTEP aims to eliminate TB in India by 2025 through strategies like improving diagnosis, ensuring appropriate treatment, preventing at-risk populations from developing TB, and strengthening related policies and resources. It outlines diagnostic protocols, treatment regimens, and initiatives to engage private providers and provide social support to patients.







![1. Park K. Park’s Textbook of Preventive and Social Medicine. 26th ed. Jabalpur: M/s
Banarsidas Bhanot; 2021
2. TB statistics India [Internet]. TBFacts. 2018 [cited 2022 Jun 28]. Available from:
https://tbfacts.org/tb-statistics-india/
3. The end TB strategy [Internet]. Who.int.. Available from:
https://www.who.int/teams/global-tuberculosis-programme/the-end-tb-strategy
4. NTEP training modules [Internet]. Gov.in. Available from:
https://tbcindia.gov.in/WriteReadData/NTEPTrainingModules1to4](https://image.slidesharecdn.com/nationaltuberculosiseliminationprogrammeautosaved-230623014946-4d00da70/85/National-tuberculosis-elimination-programme-Autosaved-pptx-57-320.jpg)
![5. Revised national tuberculosis control programme NATIONAL STRATEGIC PLAN FOR
TUBERCULOSIS ELIMINATION 2017-2025 [Internet]. Gov.in. Available from:
https://tbcindia.gov.in/WriteReadData/NSP%20Draft%2020.02.2017%201.pdf
6. Taywade M, Pisudde P. New National Tuberculosis Elimination Program (NTEP) logo:
Observation and comments. Indian Journal of Tuberculosis. 2021 Jan 1;68(1):146-8.
7. Nikshay Ecosystem Login [Internet]. Nikshay.in. [cited 2022 Jun 28]. Available from:
https://sso.nikshay.in/v1/sso/login?returnUrl=https://www.nikshay.in/Home&clientId=1](https://image.slidesharecdn.com/nationaltuberculosiseliminationprogrammeautosaved-230623014946-4d00da70/85/National-tuberculosis-elimination-programme-Autosaved-pptx-58-320.jpg)
