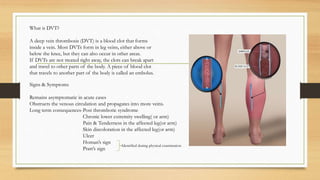
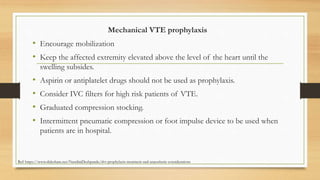
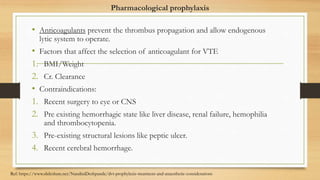
Deep vein thrombosis (DVT) is a blood clot that forms inside a vein, usually in the leg veins. If not treated, the clots can break off and travel to other parts of the body. Risk factors include genetic factors, immobilization, surgery, cancer, and oral contraceptives. Symptoms may include leg swelling and pain. Treatment involves blood thinners to prevent clot growth and embolism. Proper prophylaxis including mechanical methods and anticoagulants depends on the type of surgery and patient risk factors. Care must be taken with neuraxial procedures and indwelling catheters.




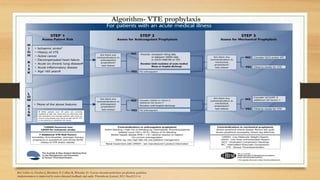
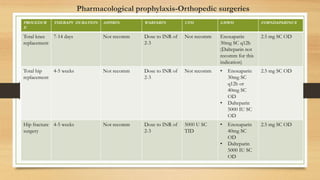


![PROCEDURE/
CONDITION
1ST LINE REGIMEN 2ND LINE REGIMEN EXTENDED
PROPHYLAXIS
Spinal surgery Offer mechanical VTE
prophylaxis on admission to
people undergoing elective
spinal surgery.
Continue for 30 days or until
the person is mobile or
discharged, whichever is
sooner.
Enoxaparin 30mg SC Q12H Post operative- Enoxaparin
30mg SC Q24H
Craniotomy SCDs alone for 30 days or
until the person is mobile or
discharged, whichever is
sooner.
Consider adding
pre-operative
pharmacological VTE
prophylaxis with LMWH.
Give the last dose no less
than 24 hours before surgery
for people undergoing
cranial surgery whose risk of
VTE outweighs their risk of
bleeding
Post operative- Consider
adding pharmacological
VTE prophylaxis with
LMWH, starting 24 to 48
hours after surgery for
people undergoing cranial
surgery whose risk of VTE
outweighs their risk of
bleeding. Continue for a
minimum of 7 days.
Pharmacological prophylaxis-Neuro surgery
Ref: Venous thromboembolism in over 16s: reducing the risk of hospital-acquired deep vein thrombosis or pulmonary embolism /NICE guideline [NG89]](https://image.slidesharecdn.com/dvtprophylaxisforsurgeries-dona-230126132426-1d02a8e4/85/DVT-PROPHYLAXIS-FOR-SURGERIES-dona-pptx-12-320.jpg)




