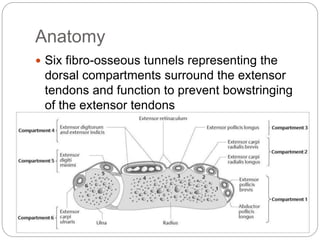
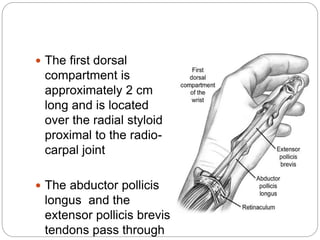
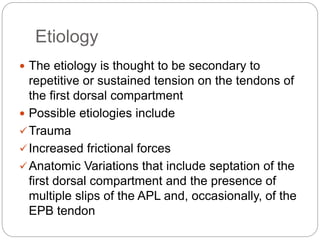
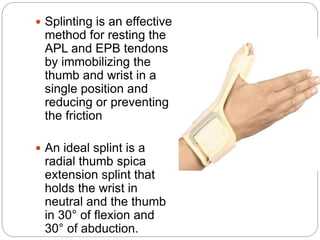
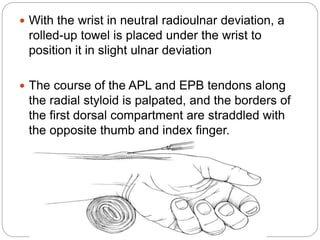
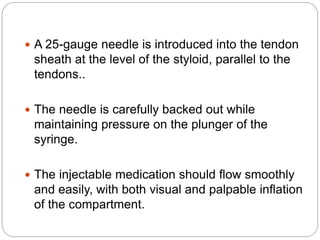
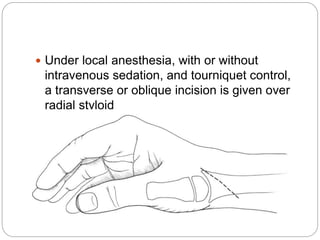
De Quervain's tenosynovitis is a condition affecting the tendons that control thumb movement at the wrist. It causes pain and swelling on the outer side of the wrist. Nonsurgical treatments include splinting, anti-inflammatory medication, and corticosteroid injections into the affected tendon sheath. If conservative treatments fail after 6 months, surgical release of the tendon sheath is recommended to relieve pressure and promote healing. The surgery involves cutting the fibrous roof of the tendon compartment to decompress the tendons.