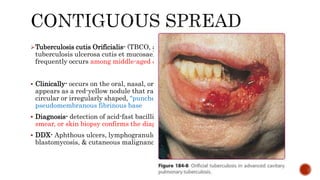
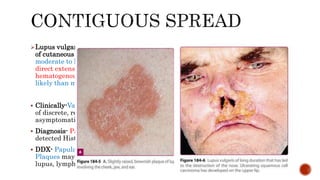
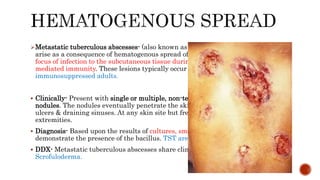
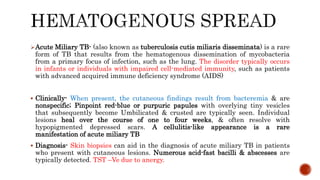
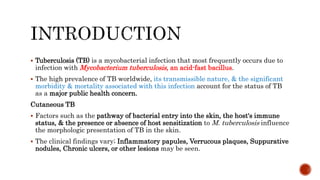
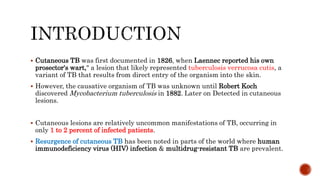
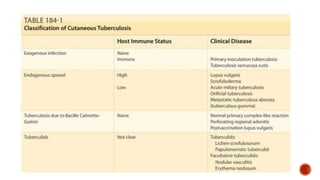
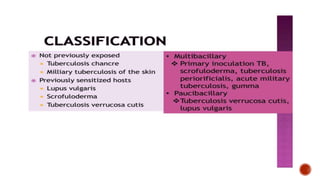
This document provides an overview of cutaneous tuberculosis (TB). It begins with objectives of explaining the pathogenesis, classifications, clinical manifestations, diagnosis, and management of cutaneous TB. It then covers the introduction, classification, clinical manifestations, laboratory diagnosis, and management approaches. Specific variants of cutaneous TB are described in detail, including primary inoculation TB, tuberculosis verrucosa cutis, scrofuloderma, tuberculosis cutis orificialis, lupus vulgaris, metastatic tuberculous abscesses, and acute miliary TB. The tuberculids, which are hypersensitivity reactions, are also discussed, focusing on papulonecrotic tuberculid and lichen scrofulo
![Beka Aberra [Internal Medicine - R2]
Dermatology Attachment
April 9, 2019](https://image.slidesharecdn.com/cutaneoustuberculosis-190415124812/85/Cutaneous-tuberculosis-1-320.jpg)
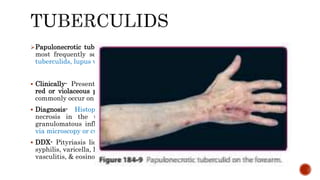
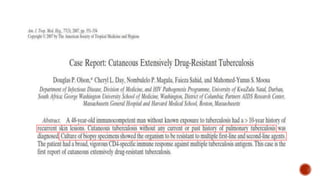
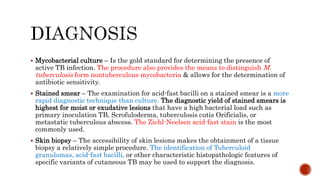
![ Similar to Extra cutaneous TB, multiple diagnostic studies are utilized for the
evaluation of patients with cutaneous TB.
The conventional techniques include
Mycobacterial culture (the gold standard for diagnosis),
Stained smears,
Lesional biopsies, &
Tuberculin skin testing.
Interferon-gamma release assays [QuantiFeron-TB GOLD]
PCR [Mycobacterial DNA in Lesional tissue]
However, in Paucibacillary variants, culture, smears, & histopathology often fail.
The Tuberculin skin test can be positive in both Multibacillary & Paucibacillary forms
of cutaneous TB; however, a positive test only identifies individuals who have been
sensitized to TB & does not confirm active TB infection.
A therapeutic trial of anti-TB medications may be used to confirm the diagnosis of TB
in difficult cases; In cutaneous TB, a response to multidrug therapy is usually evident
within six weeks.](https://image.slidesharecdn.com/cutaneoustuberculosis-190415124812/85/Cutaneous-tuberculosis-10-320.jpg)
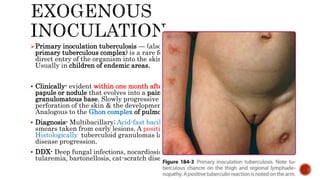
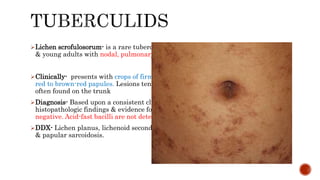
![ A characteristic histopathologic finding in Cutaneous
TB is the Tuberculoid granuloma [Low Sn/Sp], an
accumulation of epithelioid histiocytes & Langhans-
type giant cells that demonstrates a variable degree of
central caseation necrosis & a peripheral rim
composed of numerous lymphocytes.
Leprosy, tertiary syphilis, Granulomatous rosacea,
Leishmaniasis, Deep fungal infections, & other
disorders may also present with “Tuberculoid
granulomas”
Sarcoidal granulomas tend to be more circumscribed,
exhibit fewer peripheral inflammatory cells (so-called
"naked granulomas"), & are less likely to have central
caseation necrosis](https://image.slidesharecdn.com/cutaneoustuberculosis-190415124812/85/Cutaneous-tuberculosis-12-320.jpg)
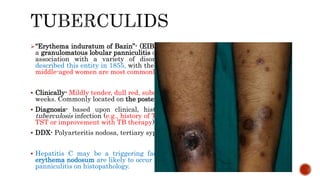
![ Tuberculin skin test – Identifies individuals sensitized to M. tuberculosis. It has a
[Sp of 63 % & a Sn 33-96 %] for cutaneous TB that becomes higher in
unvaccinated populations. The Mantoux technique, the recommended method for
performing tuberculin skin testing “delayed hypersensitivity reaction involving T
cells”. It Can be impaired in young infants, older adults, & patients with deficient
cellular immunity, “False Negatives”.
Interferon-gamma release assay – are serologic tests that assess for latent TB
infection via the measurement of interferon-gamma production from peripheral
blood mononuclear cells after exposure to antigens from M. tuberculosis.
[Sn of 92 % & a Sp of 76 %].](https://image.slidesharecdn.com/cutaneoustuberculosis-190415124812/85/Cutaneous-tuberculosis-13-320.jpg)