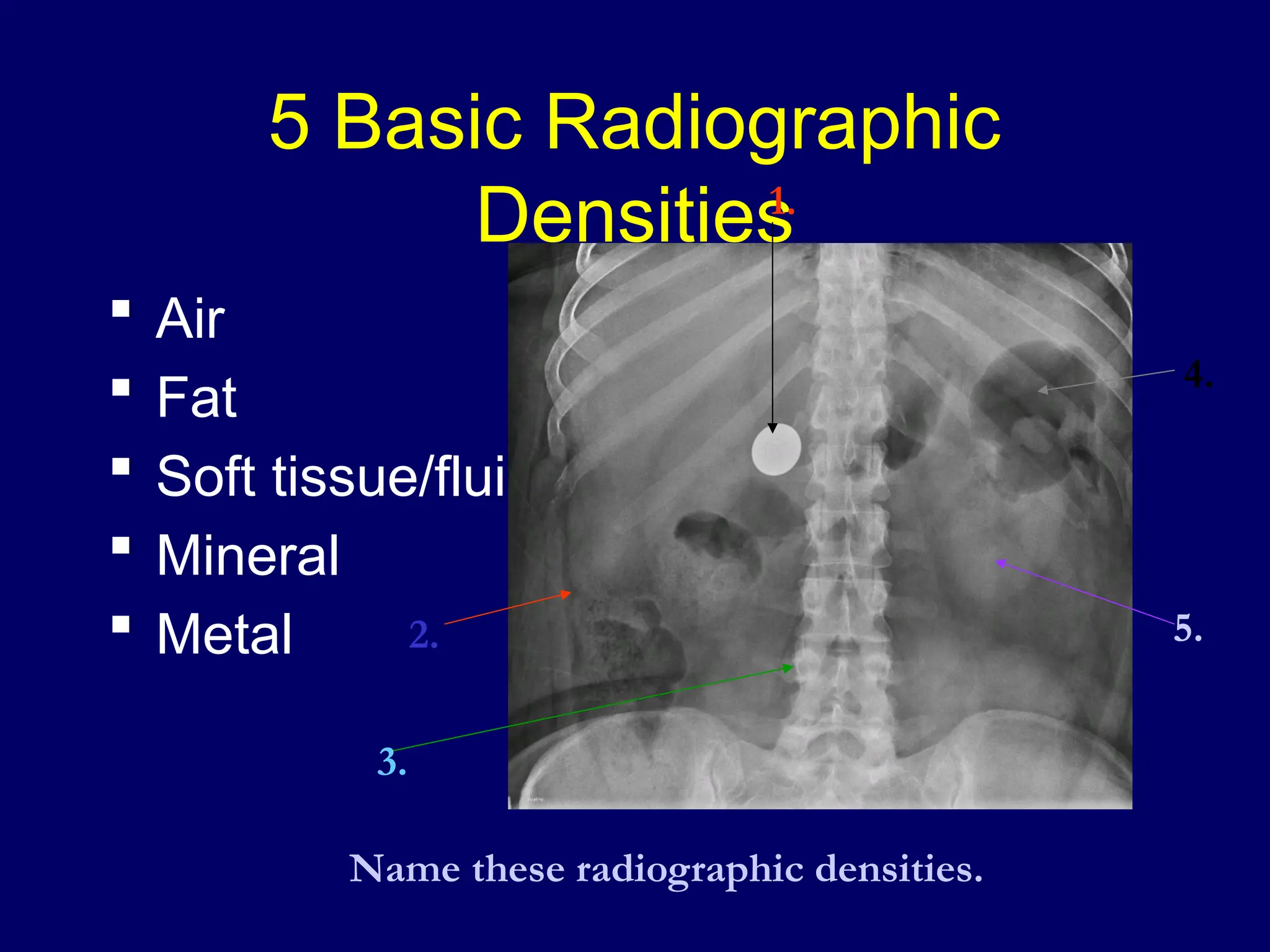
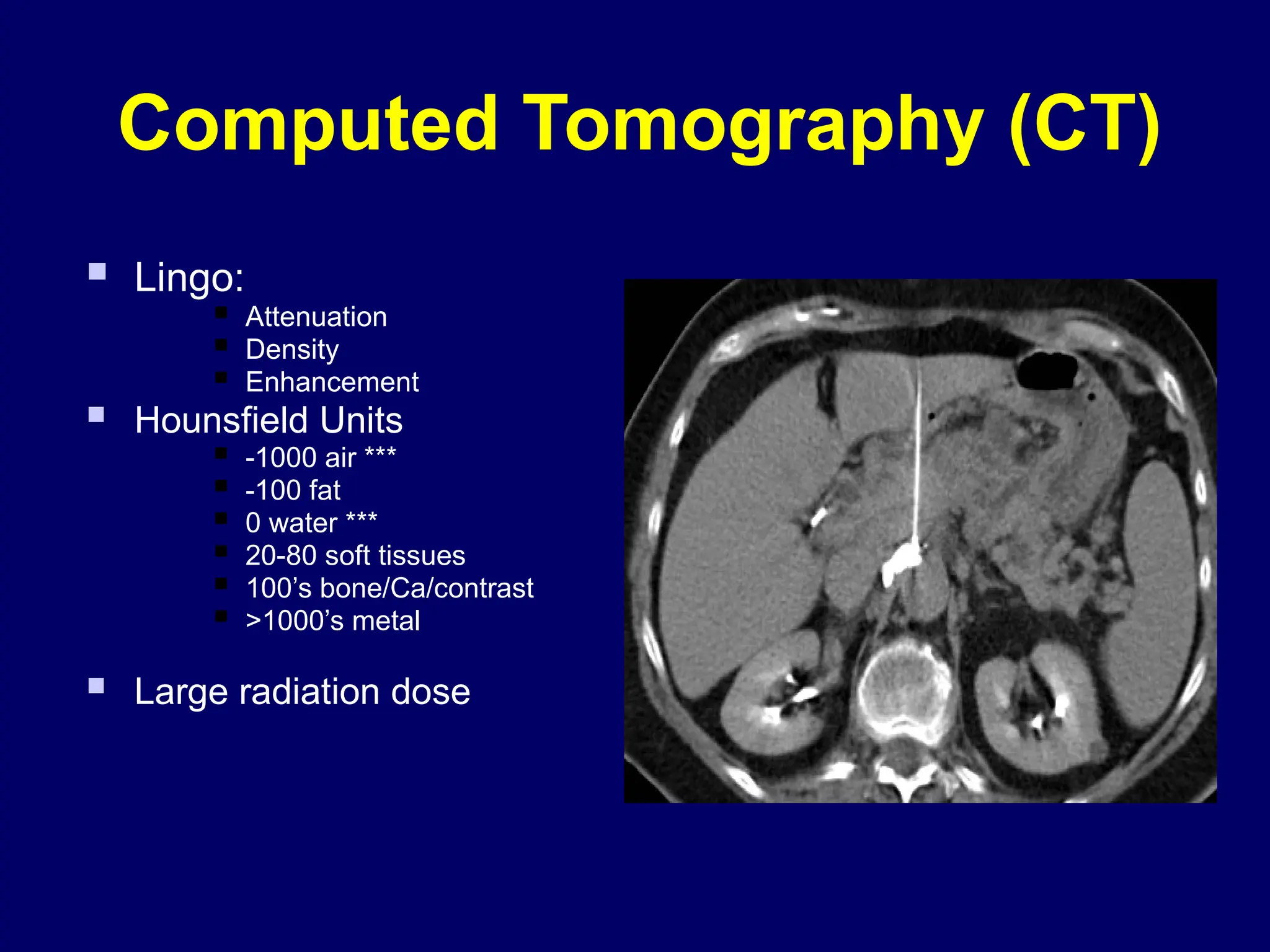
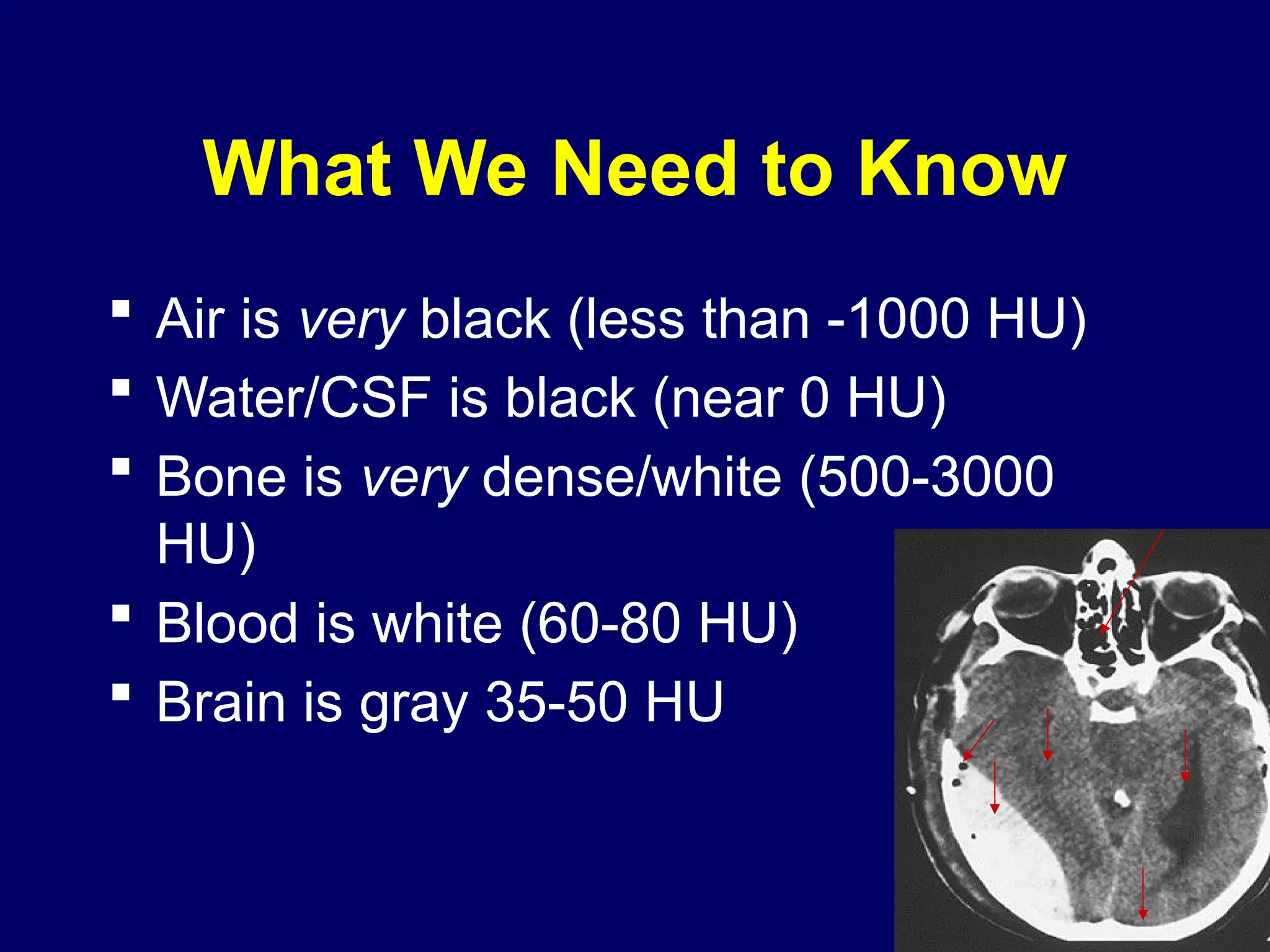
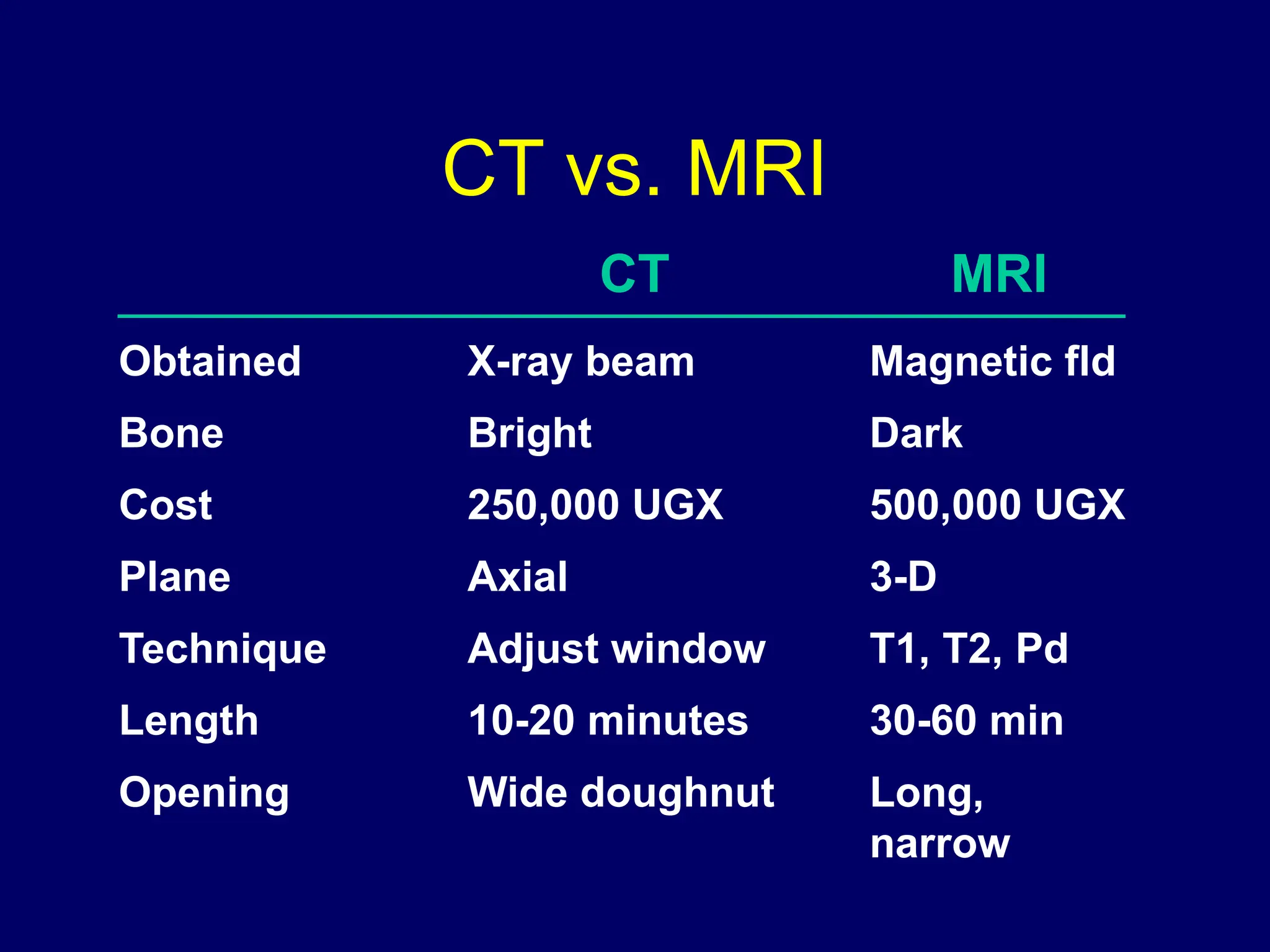
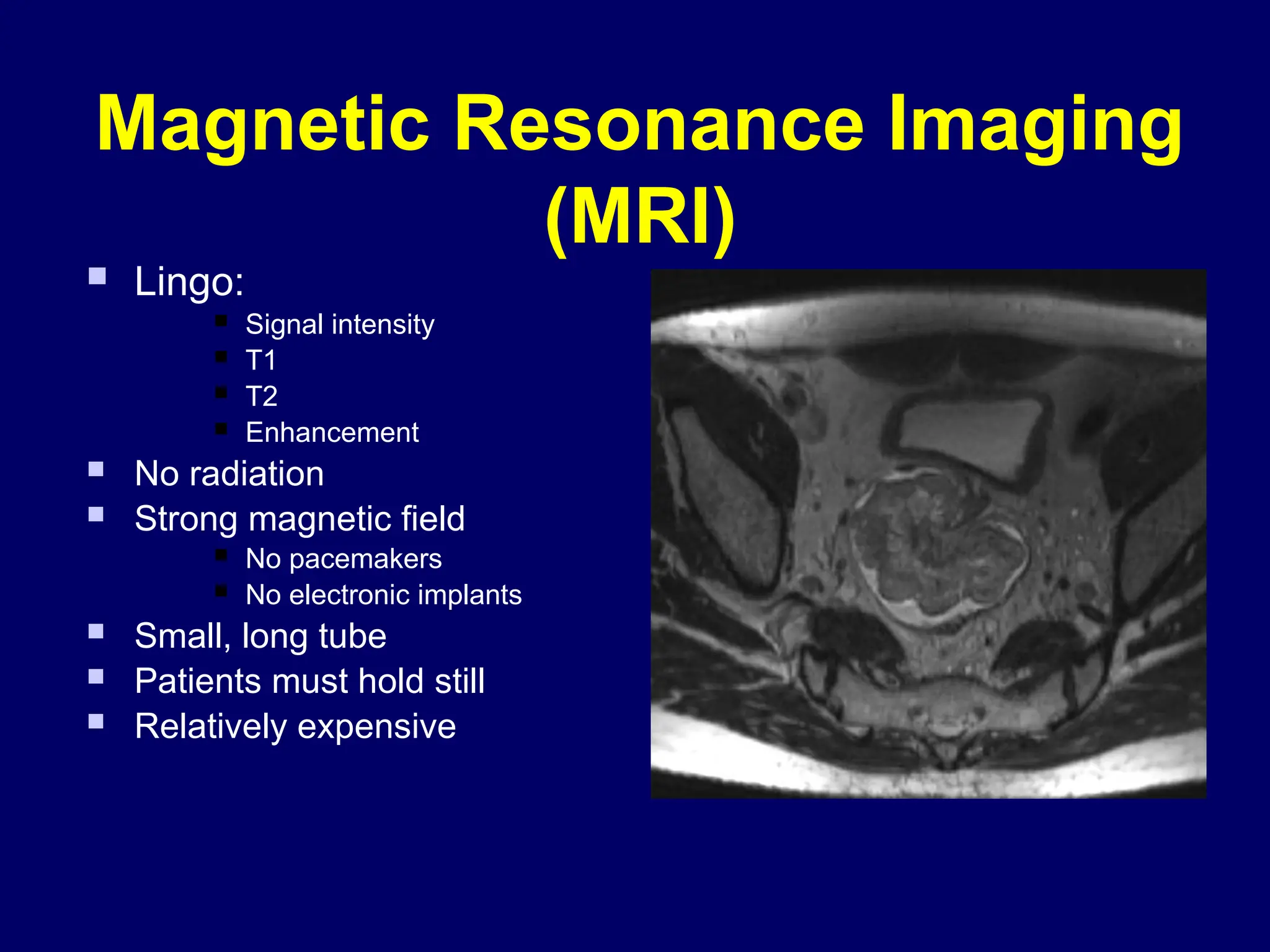
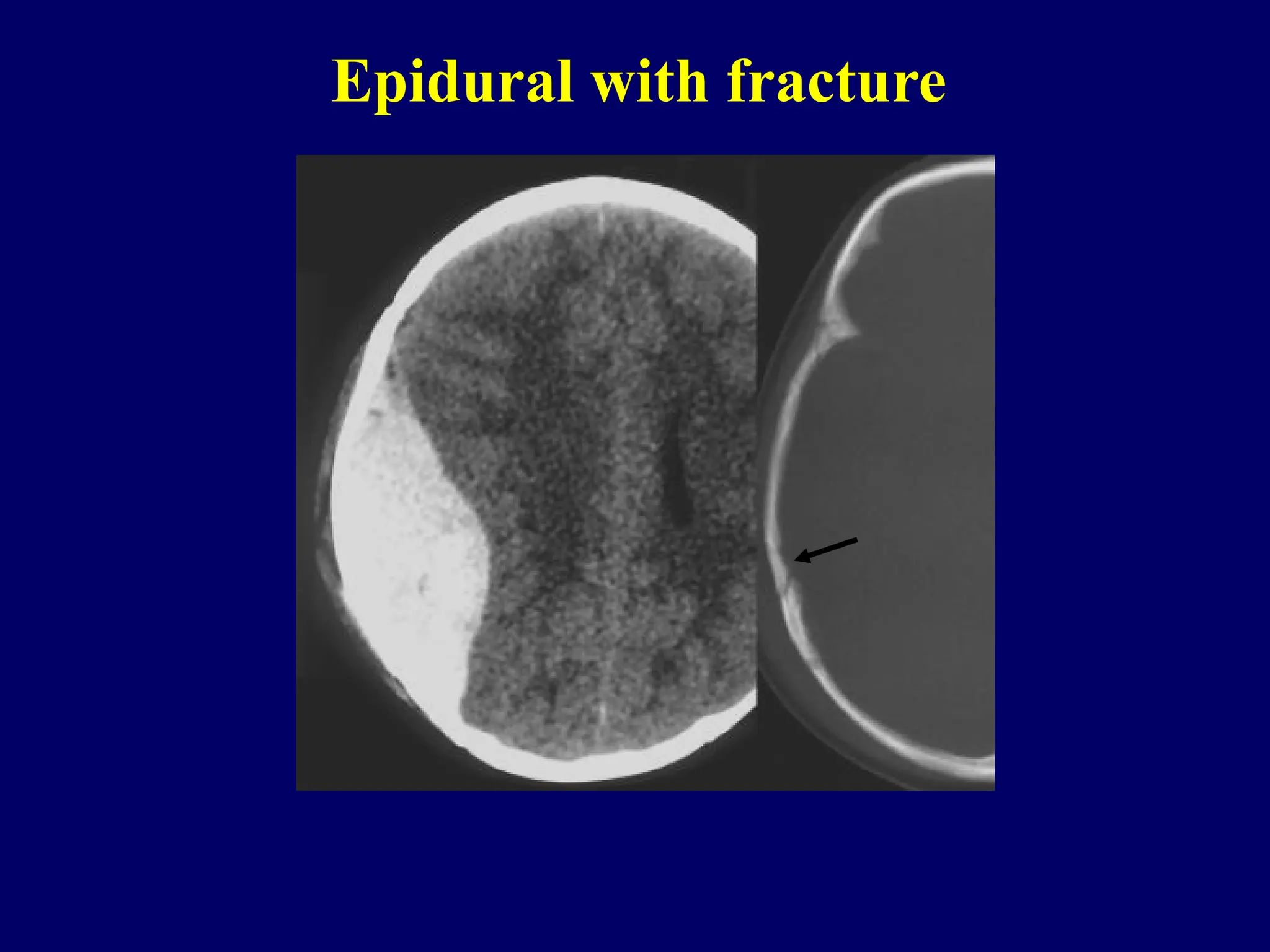
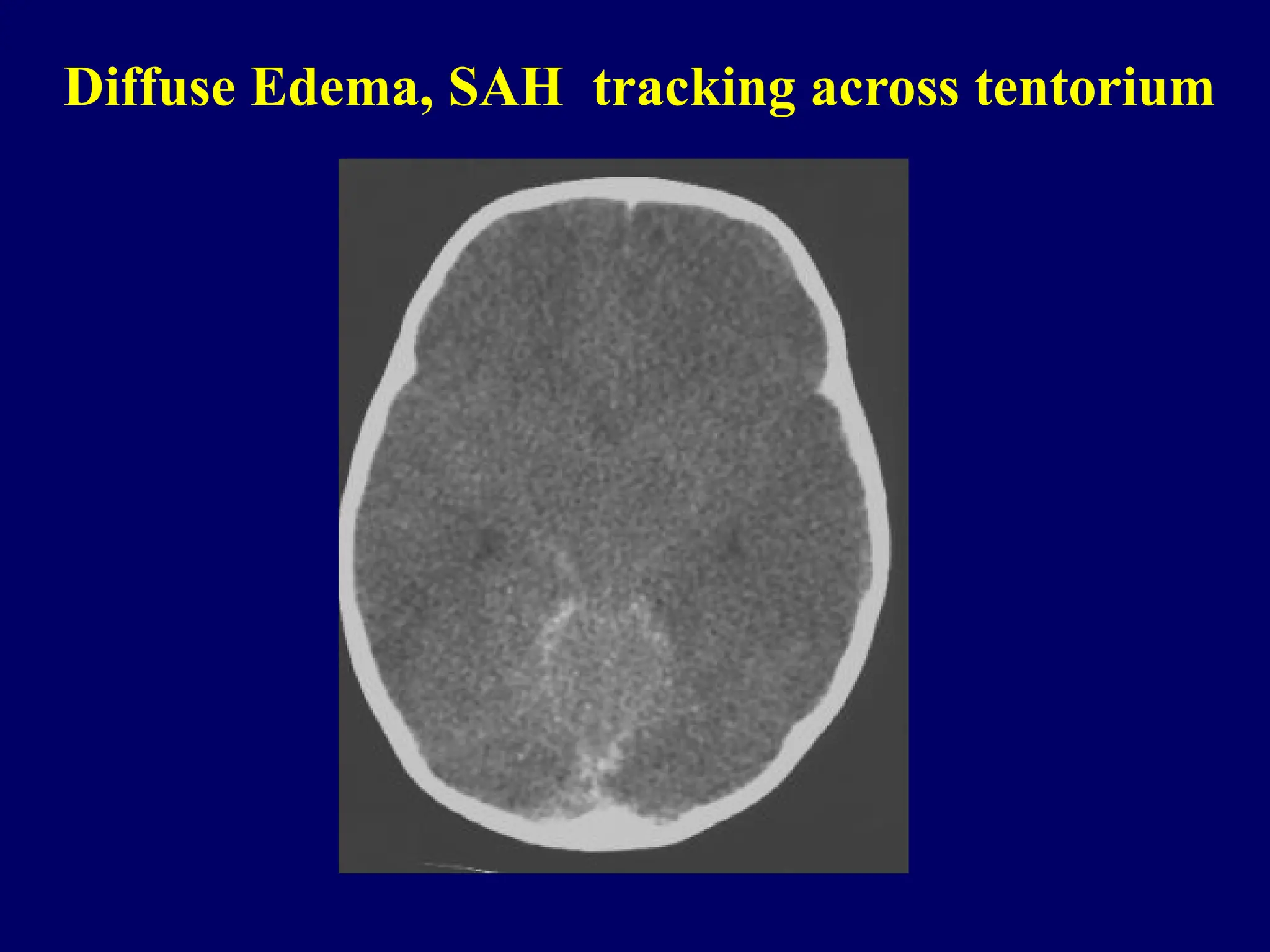
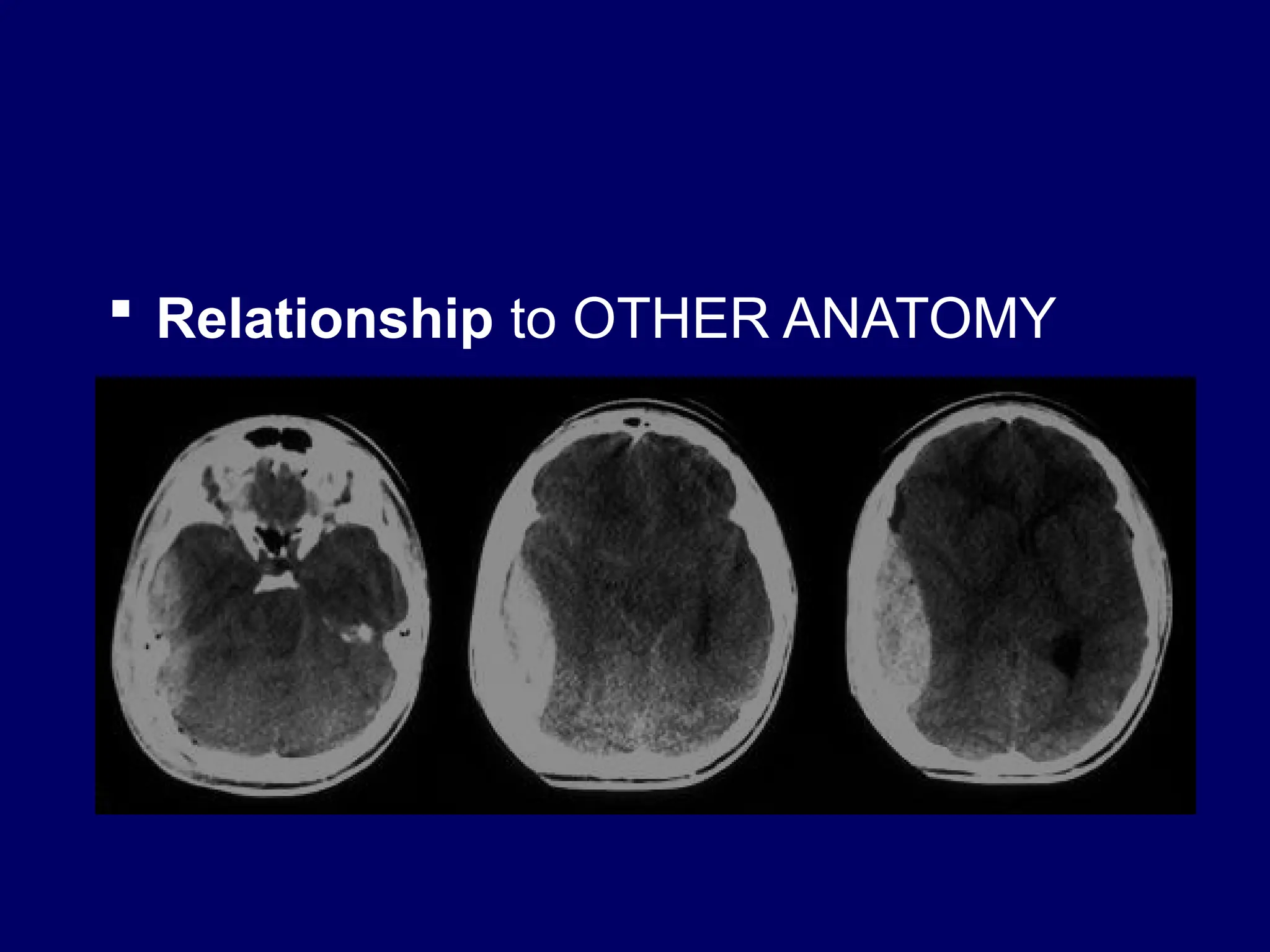
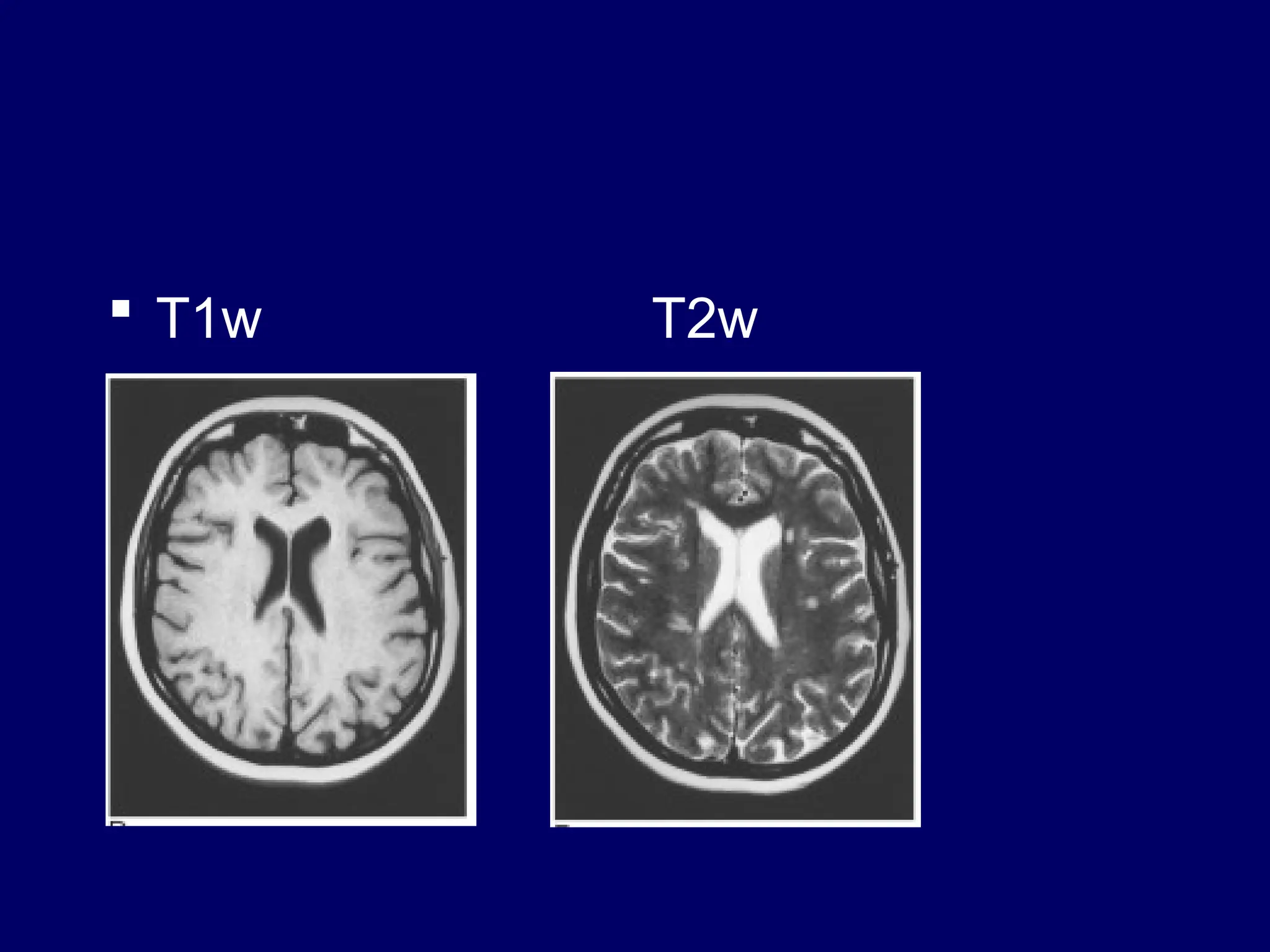
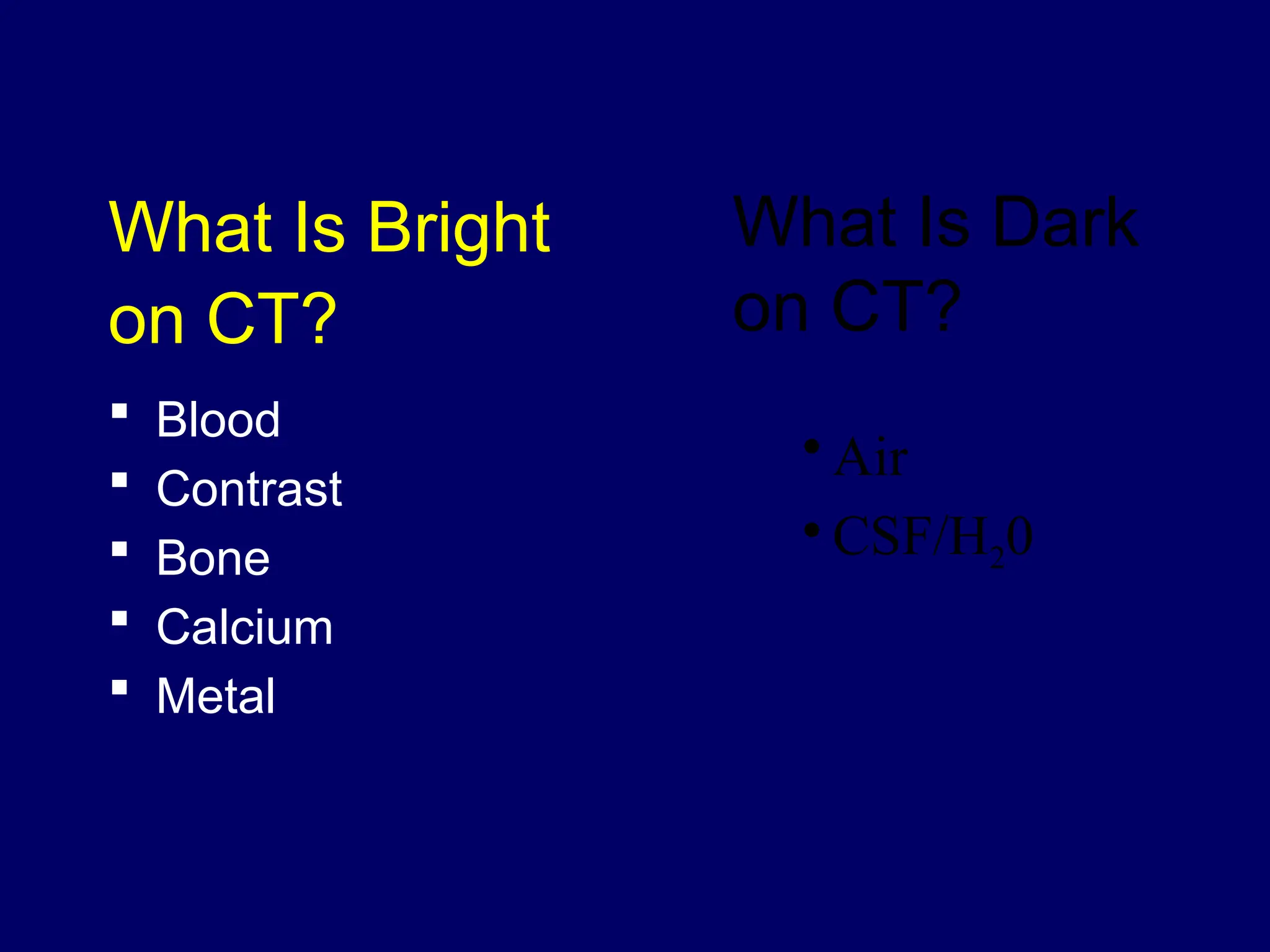
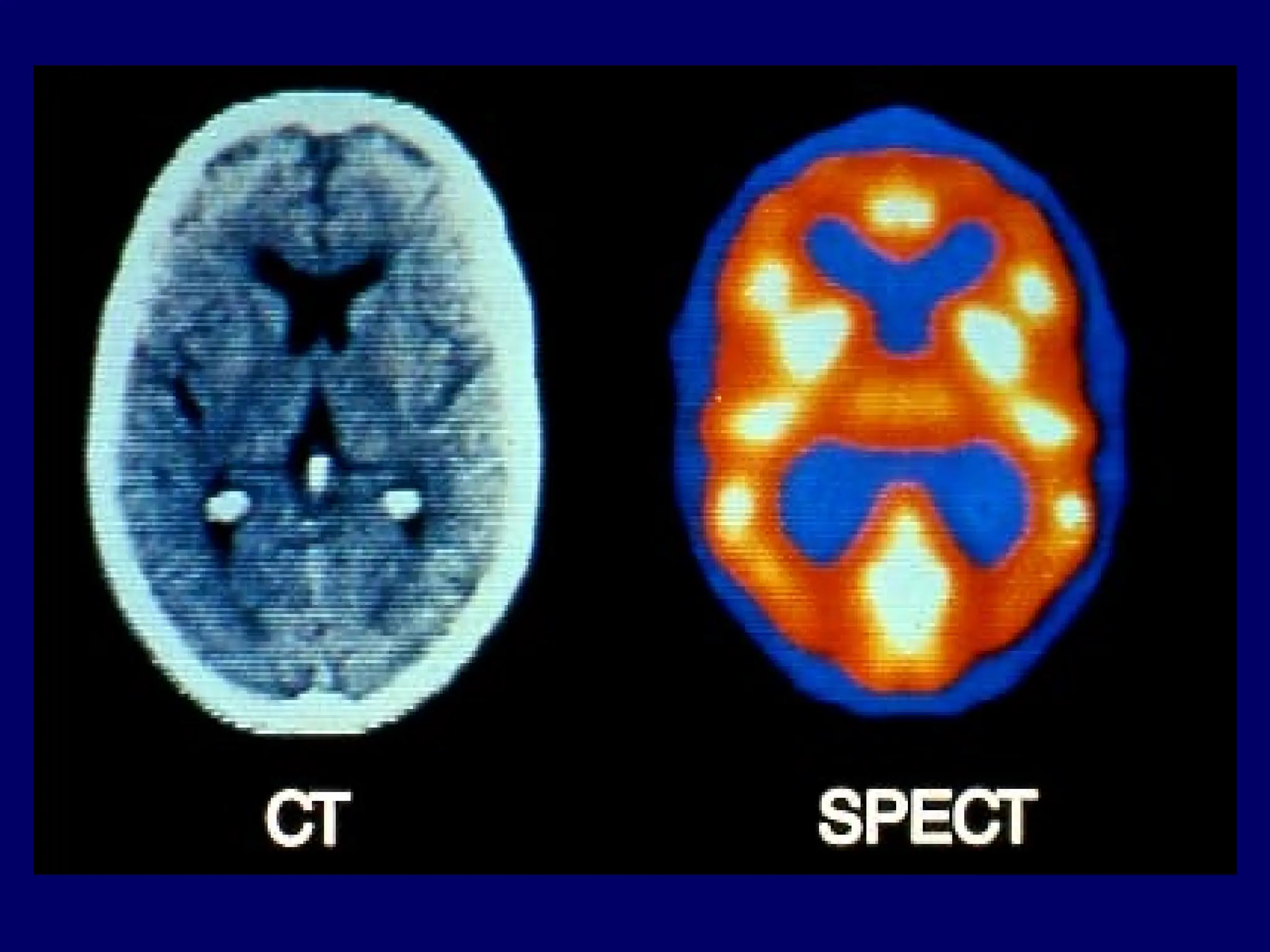
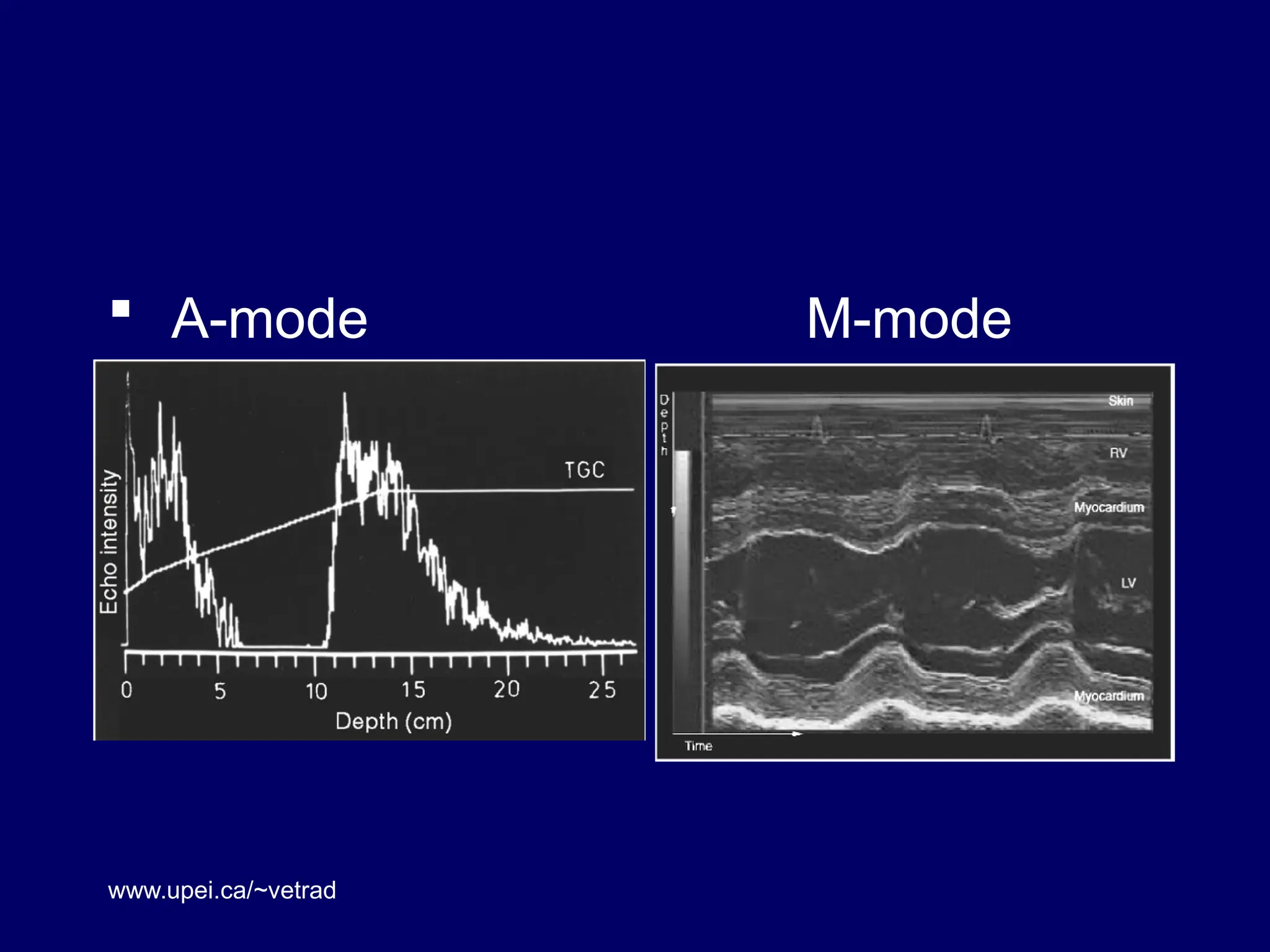
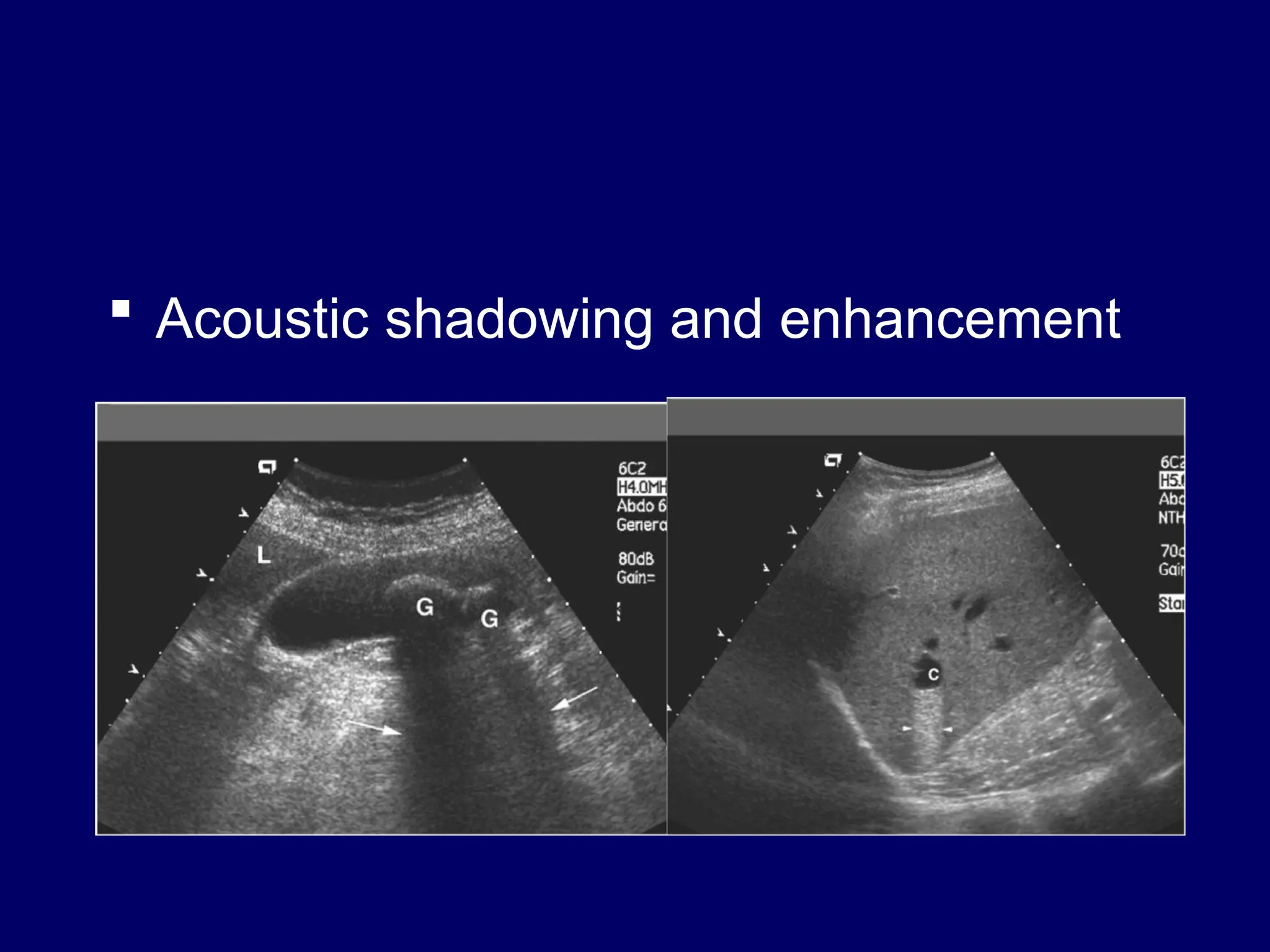
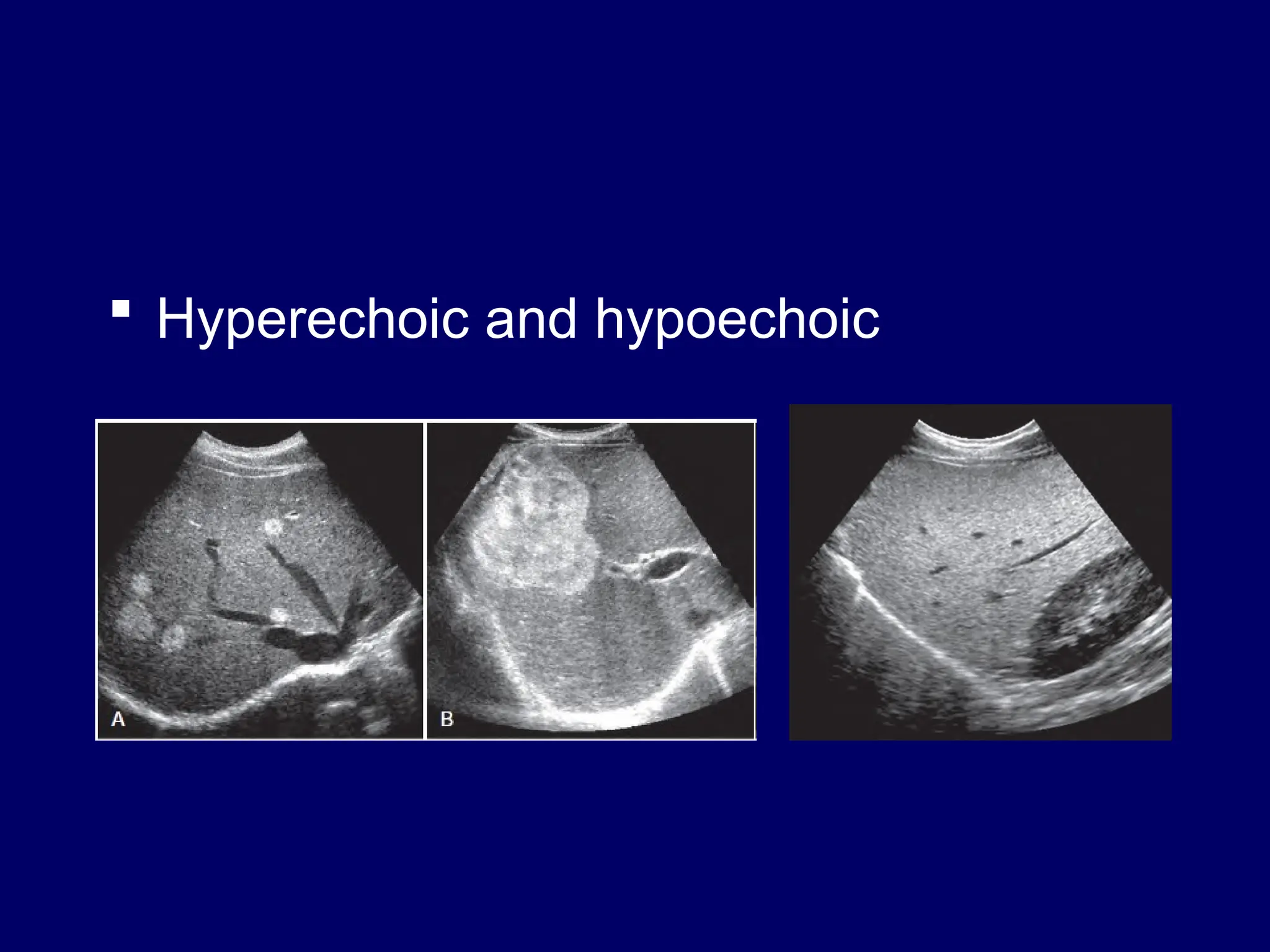
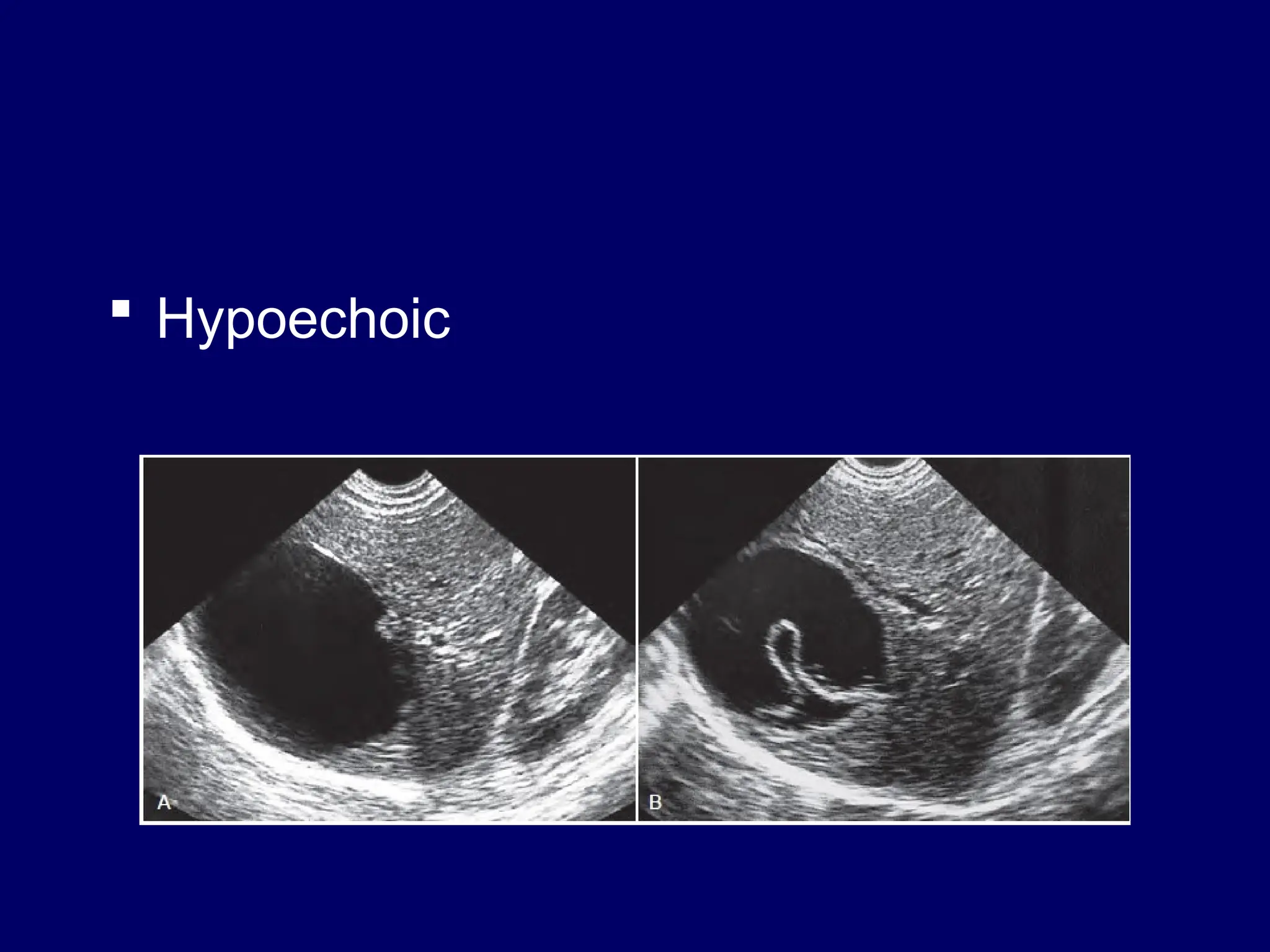
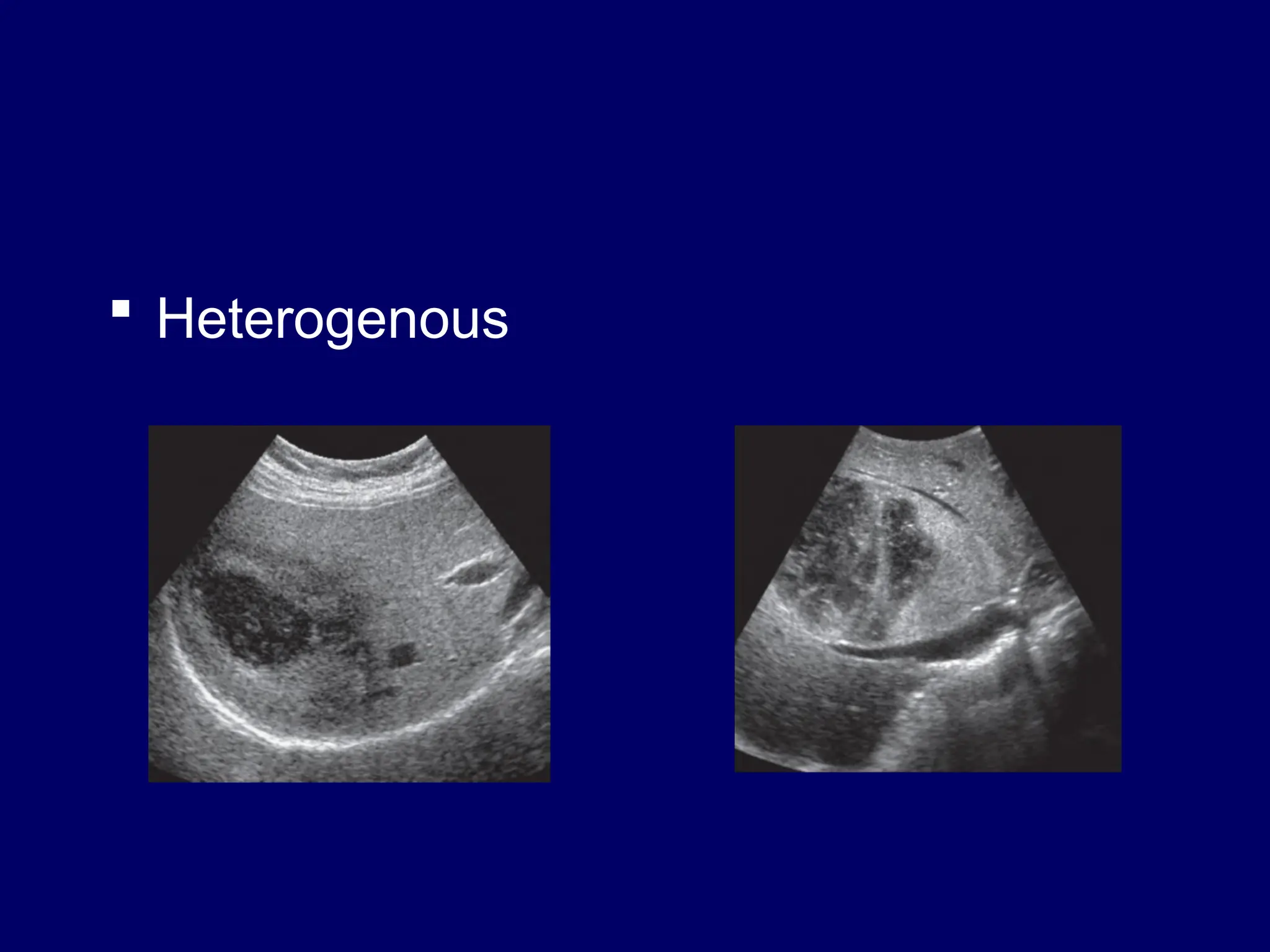
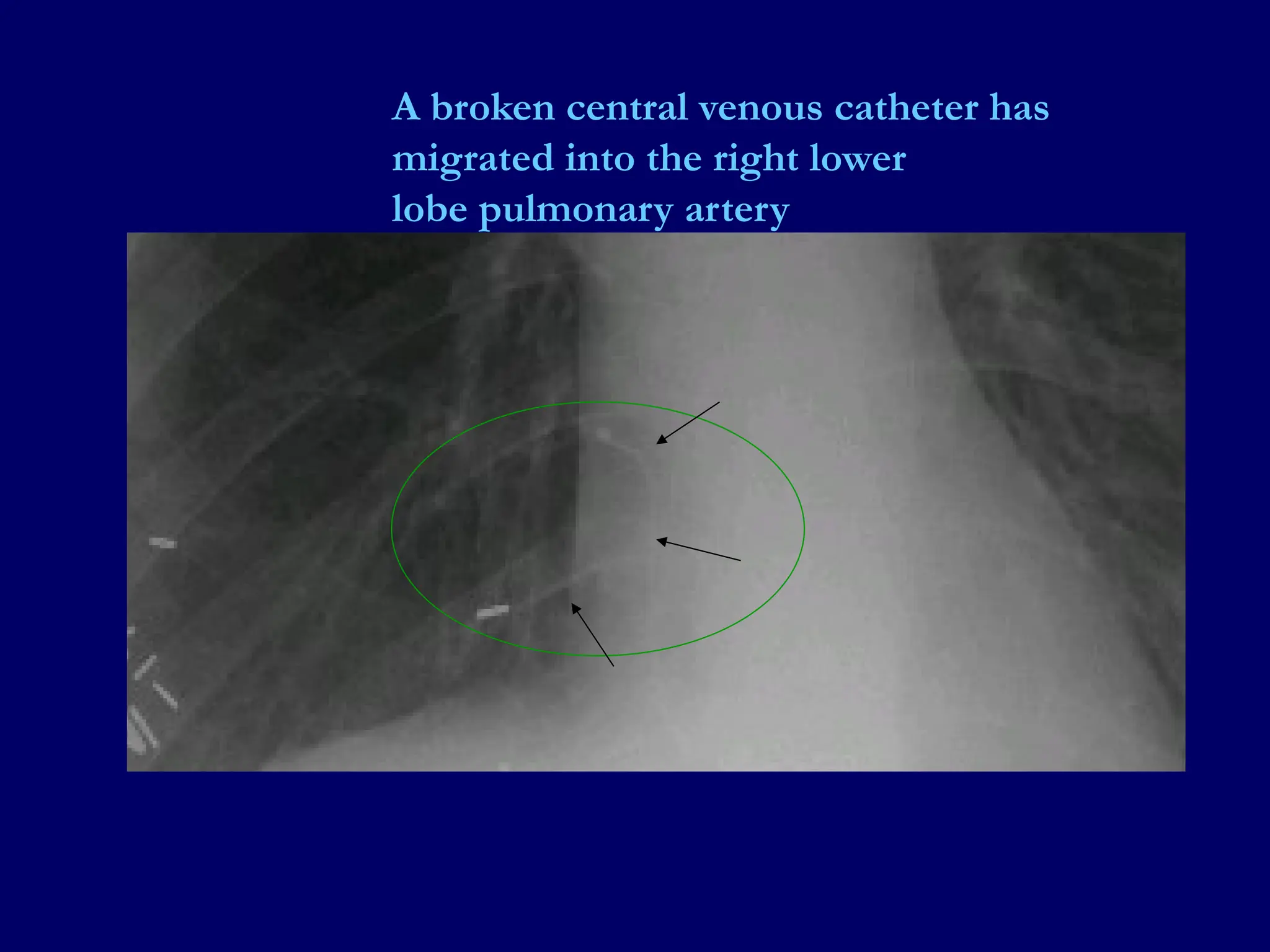
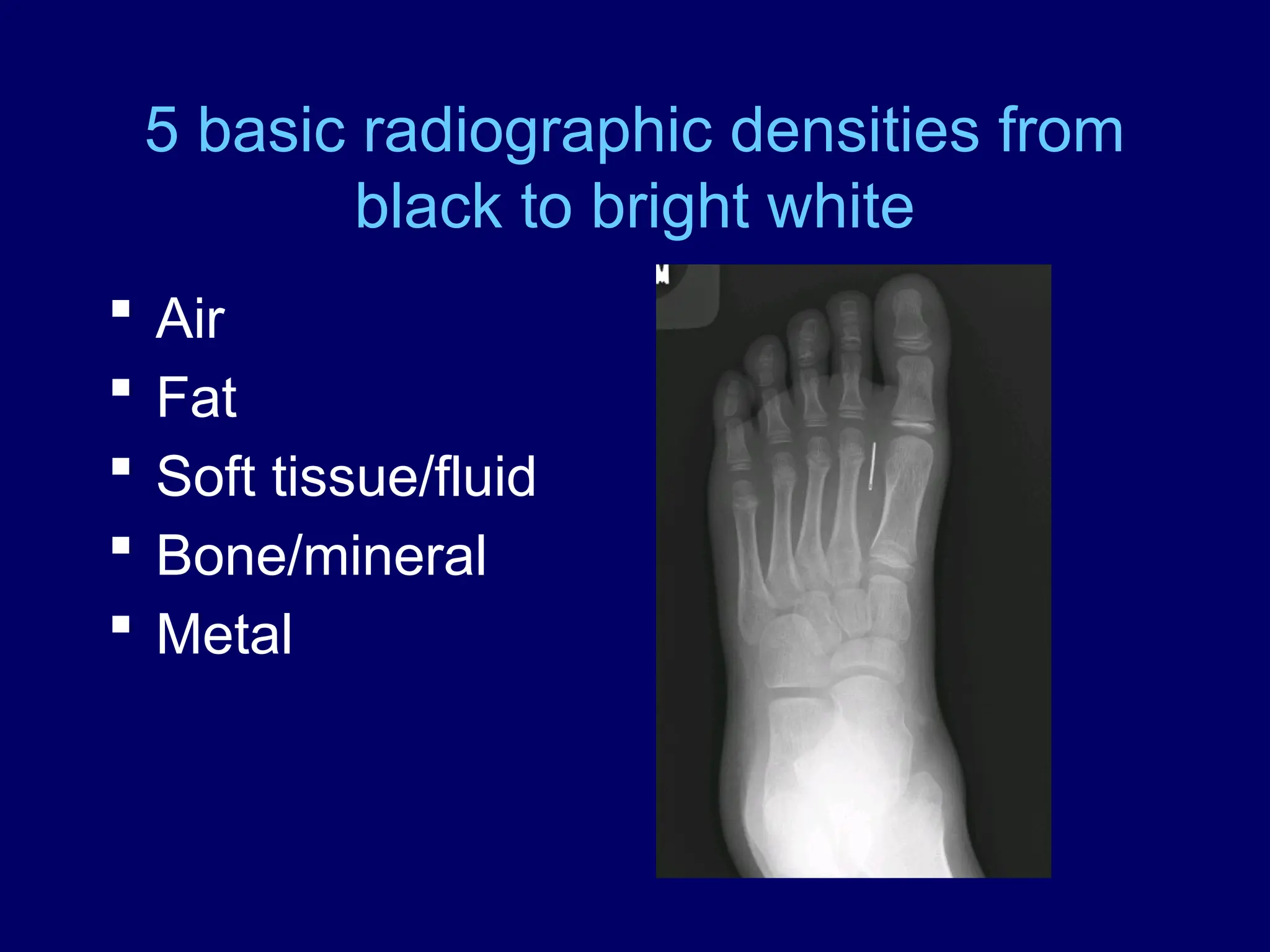
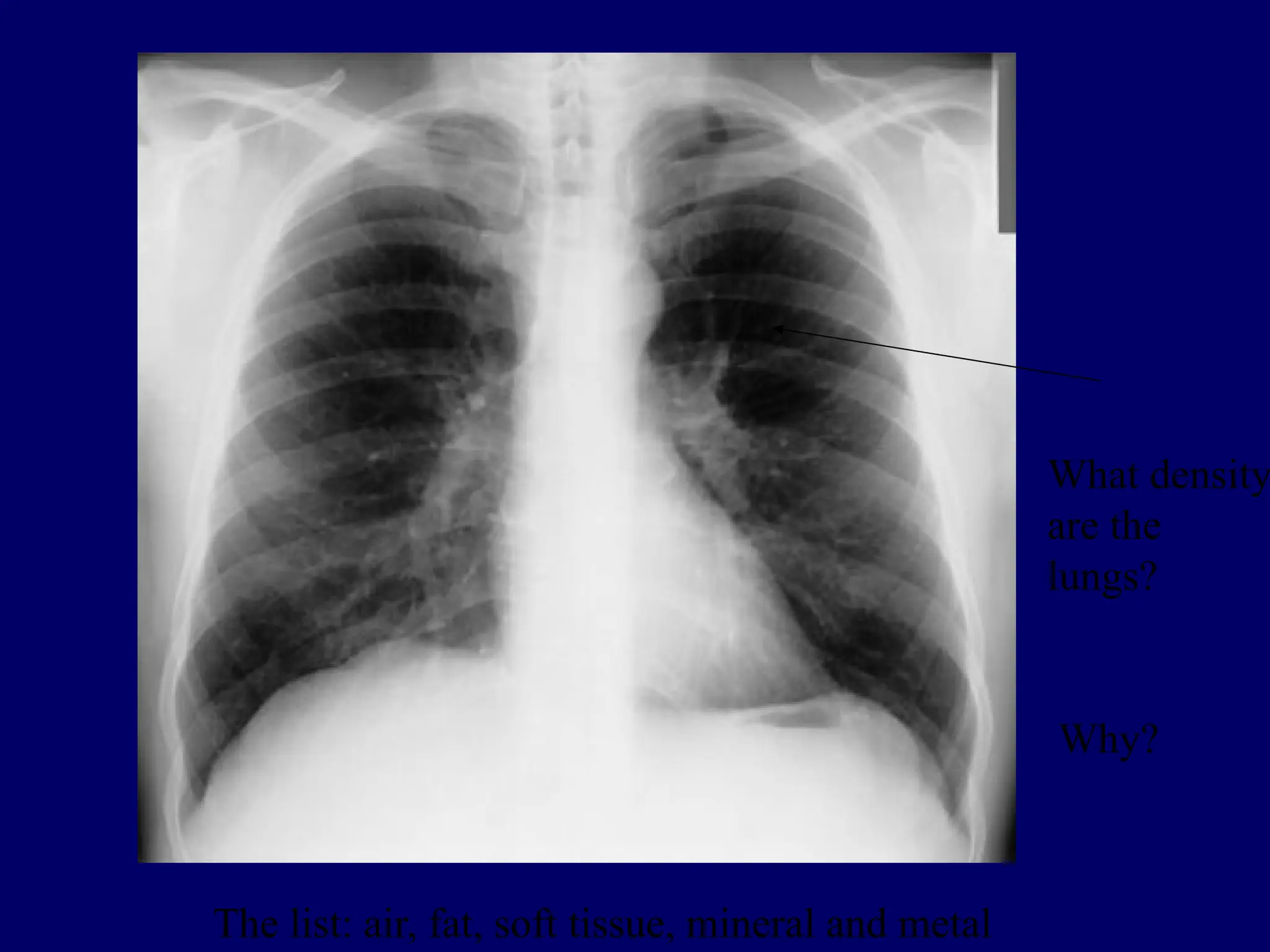
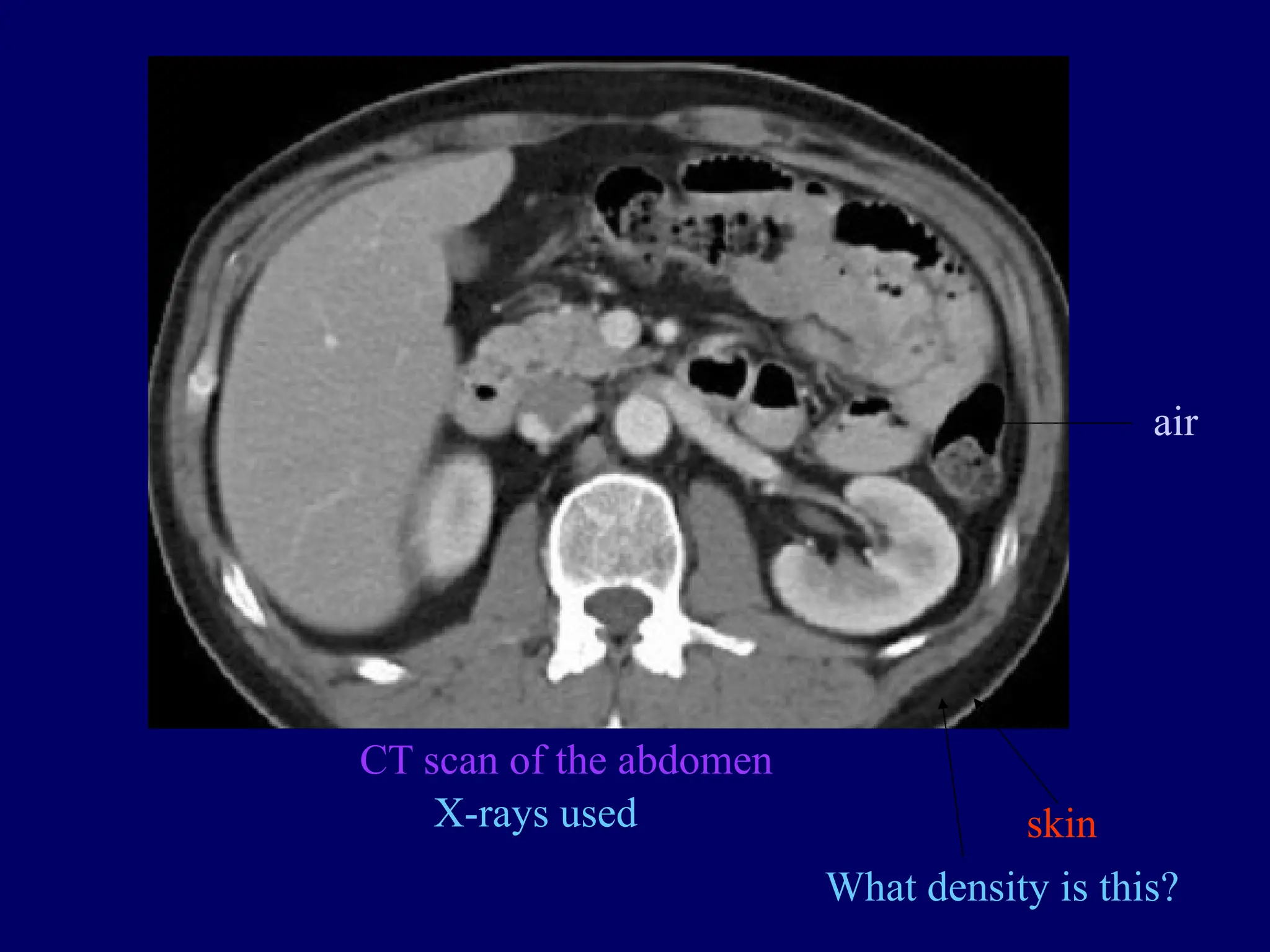
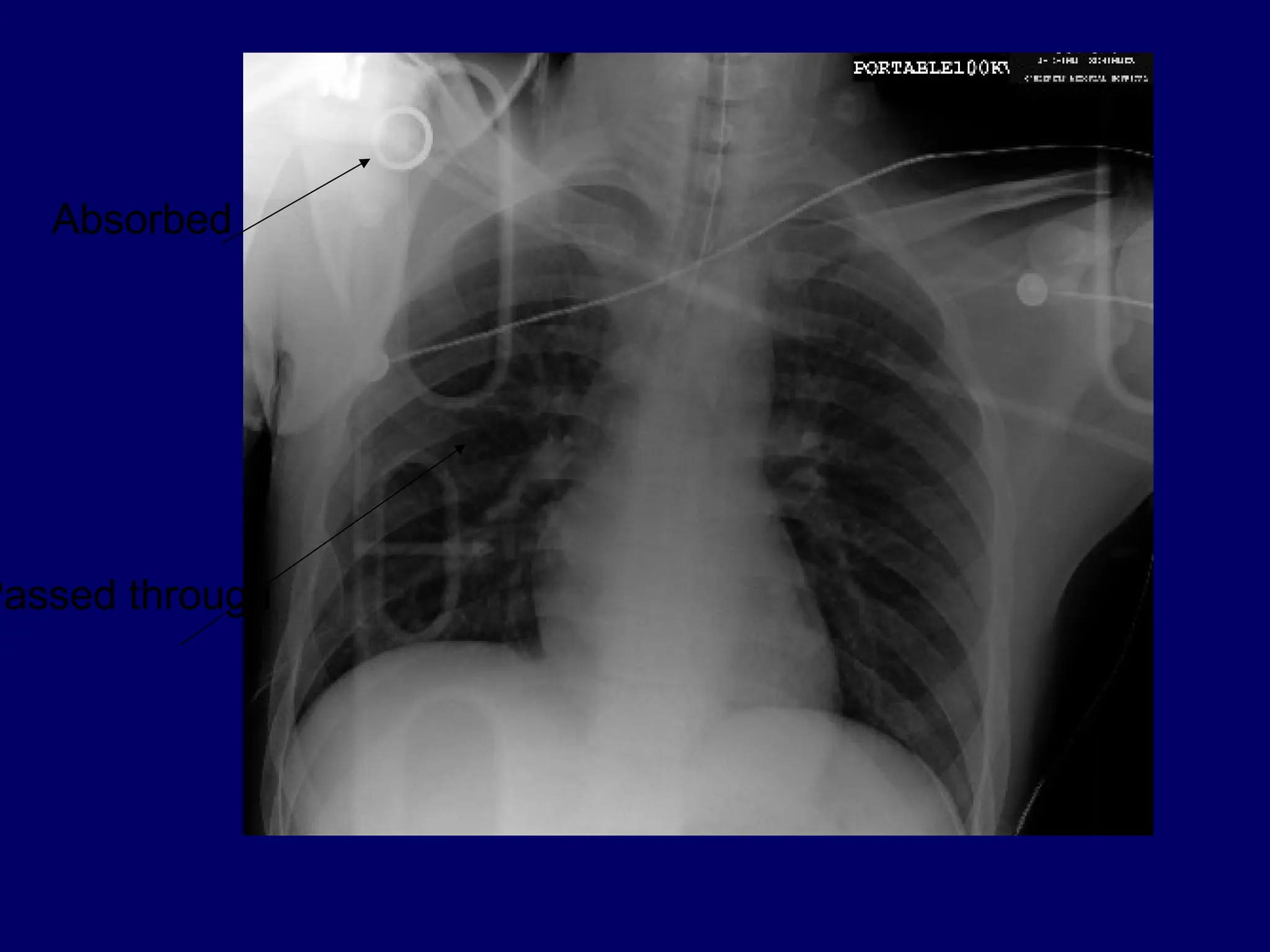
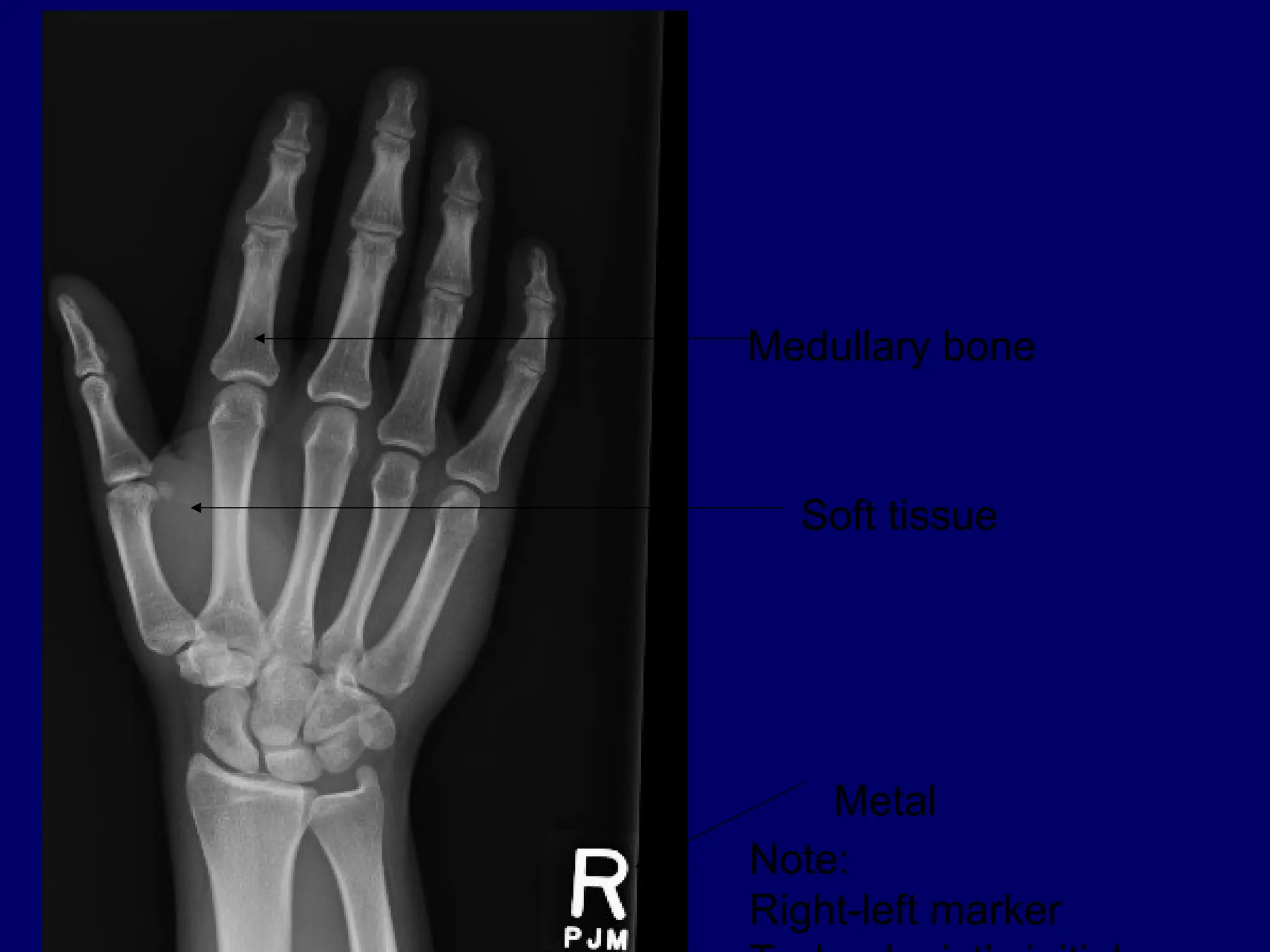
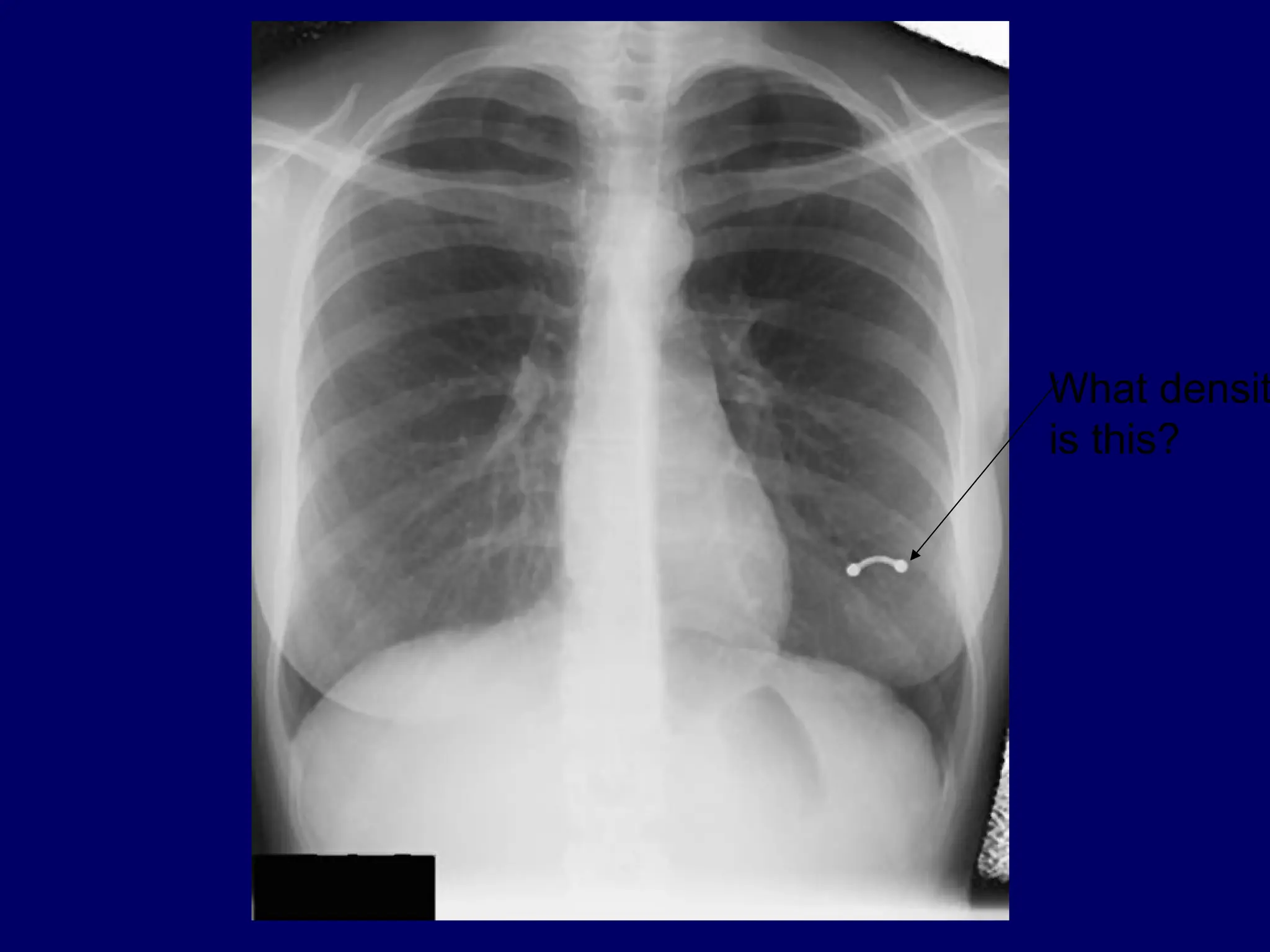
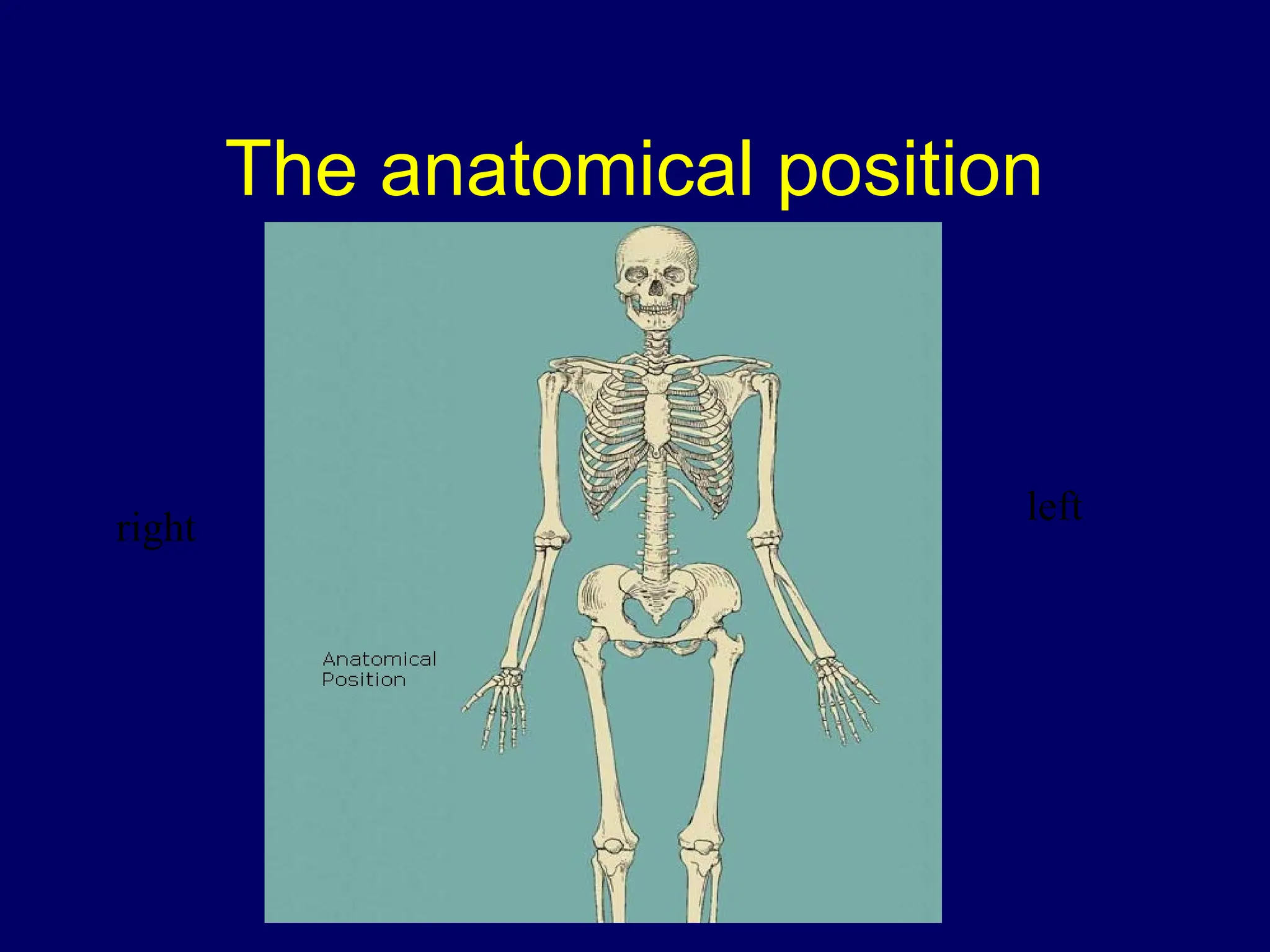
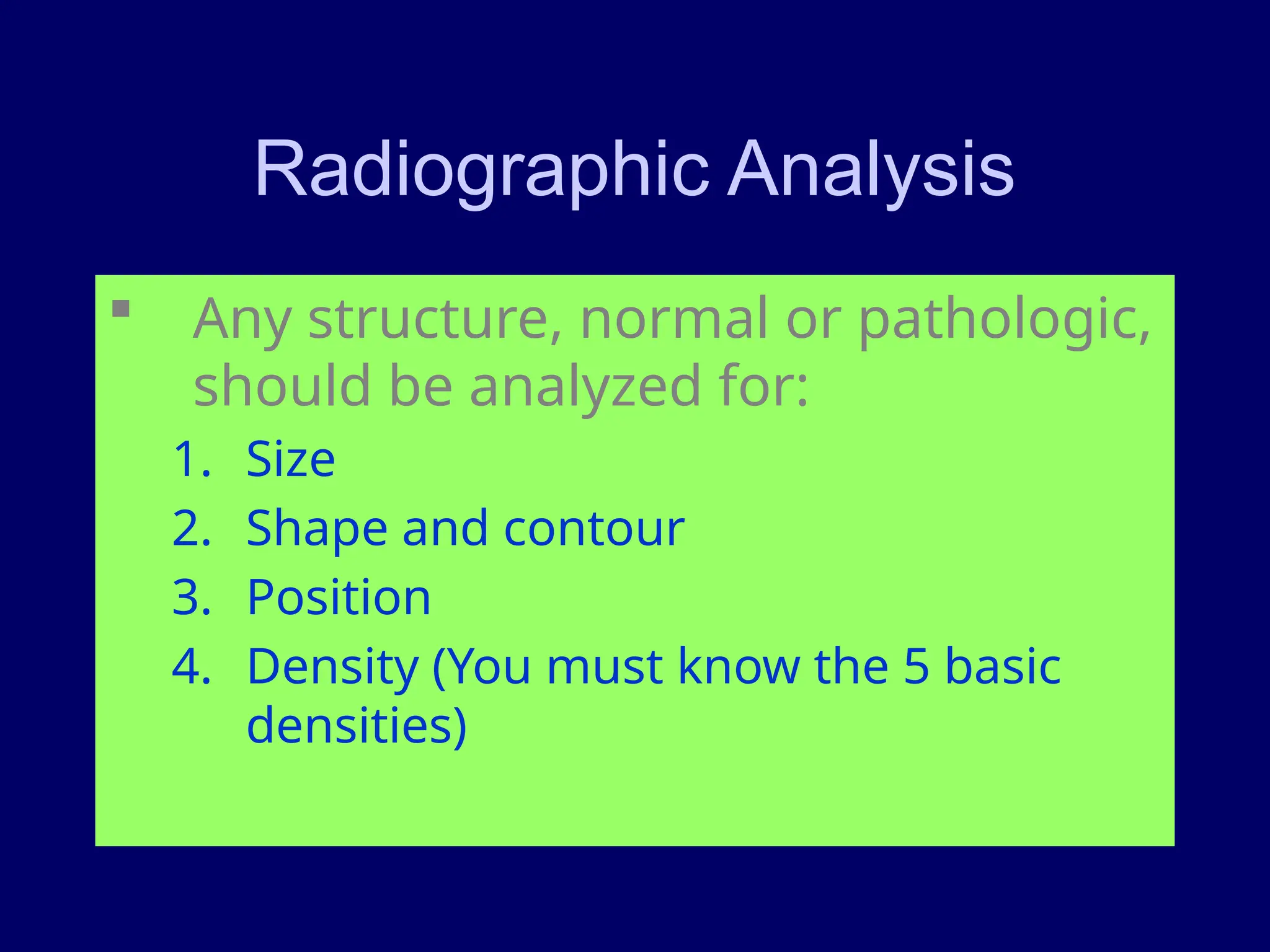
The document provides a comprehensive overview of radiological interpretation principles, including techniques for viewing images, evaluating radiographs, and understanding various imaging modalities like CT and MRI. It emphasizes the importance of systematic evaluation, knowledge of anatomy, and correlation with clinical data to avoid pitfalls in interpretation. Additionally, it discusses the differences between CT and MRI, their advantages, disadvantages, and key concepts in ultrasound imaging.