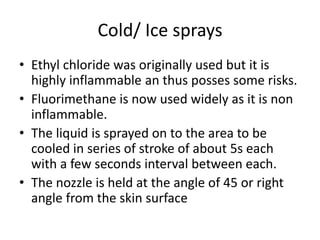
Cryotherapy uses cold to control inflammation, pain, and edema through various physiological effects. When ice is applied to skin, it conducts heat away requiring significant energy to melt. This initial vasoconstriction preserves heat for 15-20 minutes, but longer applications cause vasodilation. Cold decreases nerve conduction velocity, elevates pain thresholds, and alters muscle force generation depending on duration. Cryotherapy is used to control inflammation and edema after injuries by reducing substances like histamine. Techniques include ice packs, towels, immersion, and sprays. Contraindications include cold hypersensitivity and it should not be used over wounds or impaired healing.